What Causes Blood In Stool?
Blood in the stool (hematochezia) can be a symptom of bleeding in the gastrointestinal tract. The blood in an individual's stool may appear dark, tarry, and black, or it may be brighter red or maroon. If the origination point of the blood is higher up in the digestive tract, it is typically darker in color. Lower origination point yields a brighter, lighter, and richer color. The bloody stool may be discovered in a fecal test ordered by a physician, when wiping, or may be seen on the outside of the stool. The majority of individuals who experience this symptom will only observe mild rectal bleeding. Moderate and severe rectal bleeding may be accompanied by clots of blood and serious complications for the affected individual, including hypotension, anemia, weakness, dizziness, and syncope.
Blood in the stool can be caused by a common minor issue or could be a sign of a serious disease. Get to know the causes now.
Anal Fissures

An individual with bloody stool may be affected by anal fissures. The anus is lined with mucosa or thin, moist tissue that can become injured. An anal fissure is a term used to describe a tear in this anal mucosa. It can occur due to trauma from childbirth, chronic diarrhea, passing hard stools, anal intercourse, and straining during bowel movements. Syphilis, HIV, Crohn's disease, tuberculosis, anal cancer, and inflammatory bowel disease are some less common causes of anal fissures. Anal fissures typically present with sensations of pain, anal sphincter spasms, and rectal bleeding during bowel movements. The fissure may be visible in the skin around an individual's anus and may or may not be accompanied by a skin tag or small lump. Blood in the stool due to an anal fissure is always brighter red or maroon, as it is at the end of the gastrointestinal tract. Fresh blood that does not sit in the intestines or stomach does not have the opportunity to form grains, clots, or turn to a darker tone.
Uncover more causes behind blood in stool now.
Colon Polyps
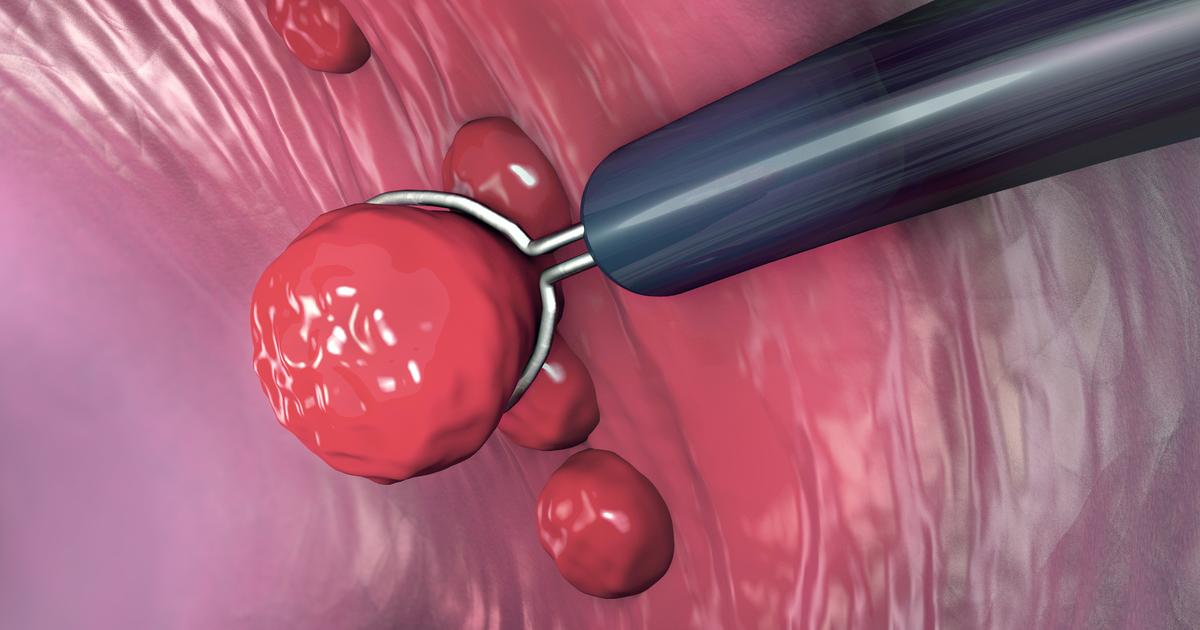
A colon polyp is a clump of cells that develops in the interior lining of the colon. Hyperplastic polyps, hamartomatous polyps, and inflammatory polyps are non-neoplastic and usually do not form malignancy. Serrated polyp types and adenomas are neoplastic polyps that have a greater risk of carcinogenesis. Polyps occur when the cells in the lining of the colon or rectum experience a DNA mutation that causes them to grow and divide inappropriately. Polyps usually do not produce symptoms until they become large and or problematic enough to cause an obstruction, inflammation, or malignancy. Due to repeated friction and irritation from passing stools, polyps may ulcerate and bleed, causing blood in the stool. While bleeding due to polyps can be associated with polyp malignancy, it does not always indicate cancer. Polyps only occur in the large intestine and rectum where the color of blood in the stool provides insight into the relative location of such polyps. Regular preventative colonoscopies can help an individual eradicate any problematic polyps before they result in serious complications like malignancy or those associated with excessive bleeding.
Read about another cause of blood in stool now.
Crohn's Disease

Bloody stools can occur due to Crohn's disease. An abnormal immune response and genetic factors are known to play a role in the pathogenesis of Crohn's disease, which falls under a category of diseases called inflammatory bowel disease because it results in digestive tract inflammation. Minor inflammation in the digestive tract is not unusual in healthy individuals, but the inflammation that occurs in those affected by Crohn's disease penetrates deep into the bowel tissue layers. The colon and ileum (last part of the small intestine) are the most prevalent parts of the digestive tract affected by Crohn's disease. Chronic inflammation of the bowel tissues caused by Crohn's disease can result in the formation of ulcers or open sores. Fistulas or ulcers that penetrate through the wall of the intestine may also develop. Anal fissures or tears in the anal mucosa are common in individuals affected by Crohn's disease. An increased risk of intestinal cancer has been proven in Crohn's disease patients. Ulcers, fistulas, anal fissures, and colon cancers that have precipitated from Crohn's disease can all produce bleeding in the gastrointestinal tract that presents as blood in the stool.
Keep reading to learn more about the reasons blood may appear in stool now.
Peptic Ulcer

The underlying cause of blood in the stool may be the presence of a peptic ulcer. A peptic ulcer describes sores that form in an individual's small intestine or stomach lining. Ulcers that develop in the stomach lining are referred to as gastric ulcers, while ulcers that develop in the upper portion of the small intestine are referred to as duodenal ulcers. Peptic ulcers form when an individual's inner stomach or duodenal lining is being eaten away by acids in their digestive tract. Healthy individuals have a mucus layer that protects the duodenal and stomach lining, but an increase in acid or a decrease in mucus can cause an individual to develop a peptic ulcer. Excessive use of non-steroidal inflammatory drugs, steroids, SSRIs, risedronate, anticoagulants, and alendronate can cause a peptic ulcer. An infection by helicobacter pylori bacteria can cause a gastric ulcer by irritating the inner stomach layer. Peptic ulcers are known to bleed and cause an affected individual to vomit red or black blood depending on the location of the ulcer. Black or tarry blood may also appear in stools. Dark coffee ground material in the stool indicates an ulcer in the stomach, where non-grainy dark blood in the stool indicates an ulcer in the duodenum.
Learn about a serious cause behind blood in the stool now.
Colon Cancer

Blood in an individual's stool can be the result of cancer that originates in their large intestine. Colon cancer is most prevalent in older adults and often starts in polyps or benign growths in the colon. Once they become malignant, growths in the colon can cause multiple symptoms associated with a slow loss of blood. Blood loss from colon cancer tends to be intermittent or comes and goes. Bright red or maroon intermittent bleeding can be attributed to a malignancy located in the rectum and last section of the large intestine. Colon cancers closer to the small intestine in the right colon have a greater risk of causing complications like anemia and low blood pressure. This type of bleeding is usually darker and may or may not be grainy. Blood in the stool and rectal bleeding that occurs due to malignancy in the lower gastrointestinal tract is most often accompanied by unusual changes in bowel habits, including abnormal consistency, diarrhea, and constipation. Unexplained fatigue, weight loss, and weakness that occur alongside blood in the stool are also commonly reported in colon cancer patients.