What Increases The Risk Of Calciphylaxis?
Calciphylaxis is an uncommon but serious disease where calcium builds up in the small blood vessels of skin and fat tissues. Often times, calciphylaxis occurs in patients who have had a kidney transplant, who have kidney failure and are on dialysis, or who have end-stage renal disease. This disease manifests in the form of skin lesions on areas of the body that contain a higher content of fat, such as the lower limbs, abdomen, buttocks, and breasts. These skin lesions do not heal and become painful nodules and ulcers. Other symptoms that occur in patients who have calciphylaxis include weakness, depression, fatigue, body aches, and cramps. This disease can be diagnosed using a biopsy of the skin, blood panels, kidney function tests, and liver function tests.
While all the causes of calciphylaxis are not known, there are numerous factors that increase an individual's risk of developing the disease. Reveal them now.
Long-Term Kidney Dialysis

Any patient being treated with long-term kidney dialysis will be at an increased risk for developing calciphylaxis. Dialysis is used to treat individuals who have kidneys that do not filter the blood effectively enough to keep waste and fluid from building up to dangerous levels in their body. This treatment is used for chronic kidney disease, short-term kidney impairment, and for patients with end-stage renal disease awaiting a kidney transplant. The way treatment with dialysis puts patients at a higher risk of developing calciphylaxis is hypocalcemia, hyperphosphatemia, hyperparathyroidism, elevated calcium-phosphorus product, and vitamin D deficiency are all very common in dialysis patients. Because dialysis is not a perfect replica of the human kidney, these types of nutrient imbalances can occur. The result is the body's metabolism of calcium and phosphorous become severely dysregulated. Because the body is unable to modulate and manage the synthesis of these nutrients in some dialysis patients, they will have a higher risk of developing calciphylaxis.
Continue reading to learn about more risk factors of calciphylaxis now.
Uremia

Uremia is a medical condition that occurs when the kidneys fail to filter the blood of wastes that would normally be eliminated through the urine. The translation of this term is 'urine within the blood.' Uremia patients will typically have increased levels of creatine, proteins, and other substances within their blood. Having this condition can significantly raise the risk of developing calciphylaxis. The way this happens is uremic toxins build up in the blood, prompting an increase of excessive reactive oxygen species (ROS) in the blood. Elevated levels of ROS in the blood vessels can result in endovascular fibrosis or the hardening and scarring of the blood vessel interior due to an overgrowth of cells. Uremia also causes a significant decrease of factors in the blood that inhibit the calcification of proteins to the inner blood vessel walls. In addition, uremia promotes the development of calciphylaxis because the excessive ROS in the blood induces an inflammatory response by the immune system. This inflammatory response has detrimental effects on the tiny blood vessels that appear in the skin and fatty tissues that are also involved in calciphylaxis.
Uncover more details on what increases the risk of calciphylaxis now.
Obesity

Obesity is characterized by an individual having too much body fat. The cause of an individual becoming obese is because they consume more calories then they use up over time. Anyone who is obese has a significantly higher risk of developing hundreds of deadly diseases than an individual who has a healthy body mass index. For the purpose of calciphylaxis, it is important to clarify the difference between an individual who is obese and one who is overweight. Overweight means an individual weighs more than what is healthy for their height. This can happen due to an excess of water, muscle, bone, or fat. Obese is defined as having a dangerously high proportion of fat tissue in the body. Because calciphylaxis develops in the fatty tissue blood vessels, individuals who are obese have a much higher likelihood of developing the disease. Individuals who have a healthy body mass index do not have much body fat for calciphylaxis to manifest itself in.
Discover more information about what increases the risk of calciphylaxis now.
End-Stage Kidney Failure

End-stage kidney failure or end-stage renal failure is the final stage of chronic kidney disease. When a patient is diagnosed with end-stage renal failure, it means their kidneys do not have enough function for them to survive without a kidney transplant or dialysis. Most patients who do qualify for a kidney transplant do not get to have one before their disease progresses into end-stage renal failure. This means the patient goes on dialysis until they are able to undergo a kidney transplant. While dialysis performs enough of the kidney's functions to keep a patient alive, it does not perform all of the functions a real kidney does. Even when a patient is being treated for end-stage renal failure with dialysis, they will still experience issues that arise due to having kidneys that do not work very good. These issues include imbalances in compounds, electrolytes, chemicals, and fluids in the body. These imbalances can trigger the development of calciphylaxis, and they do so more often when they have anything to do with calcium and phosphorous.
Learn more about what increases the risk of calciphylaxis now.
Blood-Clotting Abnormalities
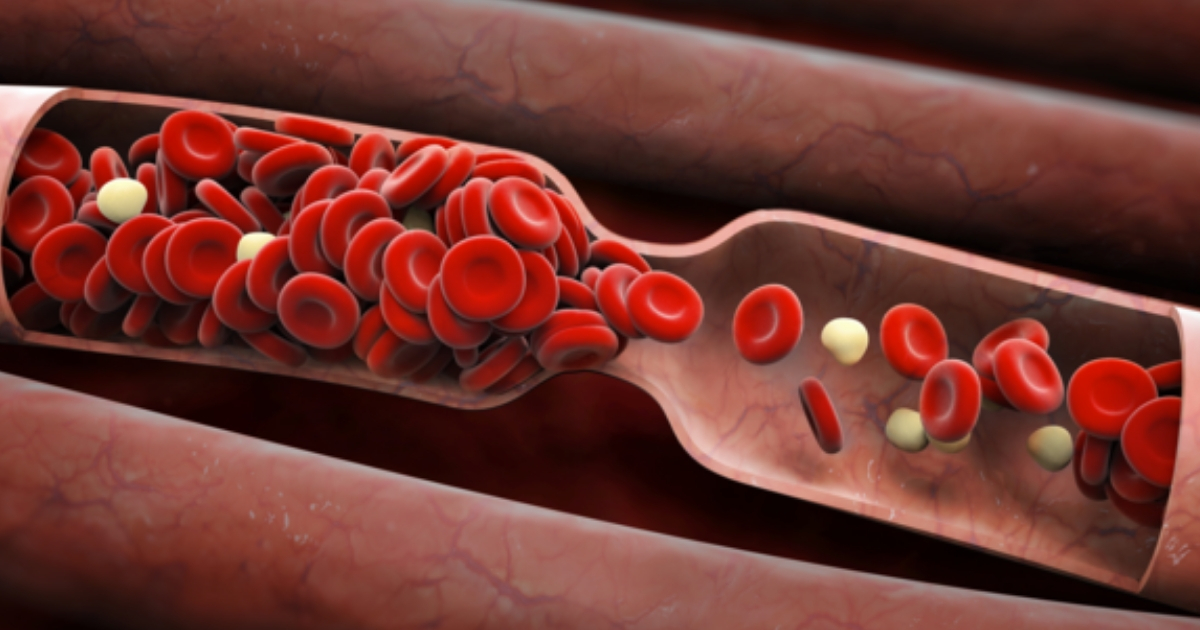
Blood-clotting abnormalities are disorders where the platelets or cell fragments within the blood responsible for clotting do not work properly. The platelets can either clot too much, or they can be scarce enough to where they are unable to form clots properly. Disorders that involve excessive clotting are the type of clotting abnormalities that can increase an individual's risk for developing calciphylaxis. This category of clotting disorders is generally referred to as hypercoagulation disorders. These disorders can be a result of several factors, including the presence of protein C deficiency, combined thrombophilia, and lupus anticoagulant. All three of these factors cause platelets to stick to each other and other tissues when they should not be. The prevalent presence of thrombophilia and lupus anticoagulant in the blood of individuals who have calciphylaxis suggests patients with hypercoagulation problems are more likely to develop the disease. The exact chemical mechanism that occurs in individuals with hypercoagulation that results in the development of calciphylaxis is not clear.