Symptoms And Progression Of Trachoma
Trachoma is a type of eye disease caused by infection with a bacterium known as Chlamydia trachomatis. The condition affects both eyes, and it is contagious, spreading from person to person through contact with infected clothing or bedding. The disease can also be transmitted through skin-to-skin contact, including handshakes, with individuals who have trachoma. Trachoma is the most common cause of preventable blindness throughout the world, and approximately two million cases of trachoma-induced blindness have been reported. The disease is prevalent in rural areas of Africa, South America, Asia, and Australia. Most cases of blindness caused by trachoma have occurred in Africa. Treatment for the condition includes antibiotics such as tetracycline and azithromycin, and these may be enough to eliminate the infection. In the later stages of trachoma, surgical intervention may be available to limit the formation of scar tissue and preserve existing vision.
The signs discussed below are some of the most frequent symptoms associated with early and late stages of trachoma.
Irritated And Itchy Eyes And Eyelids

Irritated and itchy eyes and eyelids are common in the early stages of trachoma. As the condition worsens, irritation and itchiness typically increase over time. The upper eyelids tend to be more irritated and itchy than the lower eyelids, and the upper eyelids often become thicker as irritation increases. Swelling of the eyelids is frequently seen, and the eyelids and eyelashes may turn inward during the late stages of the infection, scratching the cornea and intensifying irritation. Eye specialists can evaluate the severity of any irritation and the potential for eye damage, and they may be able to prescribe certain eye drops that could reduce itching and calm inflammation. For trachoma patients whose eyelashes have started to rub on and irritate the cornea, a surgical procedure called epilation might be considered. This procedure removes the lashes. If this operation is not available in the patient's location, doctors usually recommend placing an adhesive bandage over the eyelashes to prevent them from touching the eye.
Uncover more symptoms of trachoma now.
Eye Discharge And Pain

Eye discharge and pain may happen at any stage of trachoma. The discharge seen in this particular illness normally consists of pus. Since trachoma frequently occurs in crowded areas with low levels of sanitation, it may be difficult to control or treat the discharge. If possible, a bandage should be placed over the eyes to prevent discharge from infecting others, and patients and caregivers should avoid touching the eyes or items that have been in contact with the discharge. Patients with advanced trachoma and those who have had repeated infections with the bacteria will likely experience changes to the lacrimal glands of the eyes. These glands produce tears that moisten the eyes, and the changes caused by trachoma could stop them from working properly, decreasing moisture in the eye and resulting in extreme dryness that could increase pain. Lubricating eye drops and pain relieving ointments may be useful in keeping patients with trachoma more comfortable.
Continue reading to reveal more warning signs of trachoma now.
Light Sensitivity

Patients with trachoma may have varying degrees of light sensitivity, which is also known as photophobia. The eye discharge, corneal scarring, and inflammation of the upper lid that occur with the disease could all make light sensitivity worse. To manage this sensitivity, patients should use any eye drops they have been prescribed, and they may wish to use artificial tears to decrease dryness that could trigger the sensitivity as well. Staying in a dark room is not recommended. Instead, experts suggest gradually increasing exposure to light. In addition, patients may need to take steps to reduce glare and reflection inside their living spaces. For example, reflective or shiny surfaces that can cause intense light sensitivity can be covered with a towel or sheet, and cleaning counters and mirrors will reduce streaks that may also contribute to glare. For patients who wear glasses, tinted lenses may be available for protection from potentially painful kinds of light wavelengths, and it may be necessary to wear sunglasses with polarized lenses while outdoors. Some patients with photophobia may also have depression or anxiety, and speaking with a mental health professional may improve symptom management.
Learn more about symptoms of trachoma and their progression now.
Progression Of Inflammation

The inflammation that occurs with trachoma is divided into stages. In the first stage, known as follicular inflammation, an eye specialist will see at least five follicles on examination with magnification. Follicles are tiny bumps that contain white blood cells, and they will be visible on the conjunctiva, the inner surface of the eyelid. As the inflammation continues to the second stage, intense inflammation will be observed. The upper eyelid will be thicker than normal, and swelling will also be present. If the patient has had trachoma for a long time, the inflammation may produce scars on the inside of the upper eyelid. These scars typically appear as white lines when viewed under magnification. As inflammation progresses, the inner part of the eyelid becomes deformed, and both the eyelid and the upper lashes could turn inward, a condition known as entropion.
Get more details on the symptoms of trachoma now.
Corneal Clouding
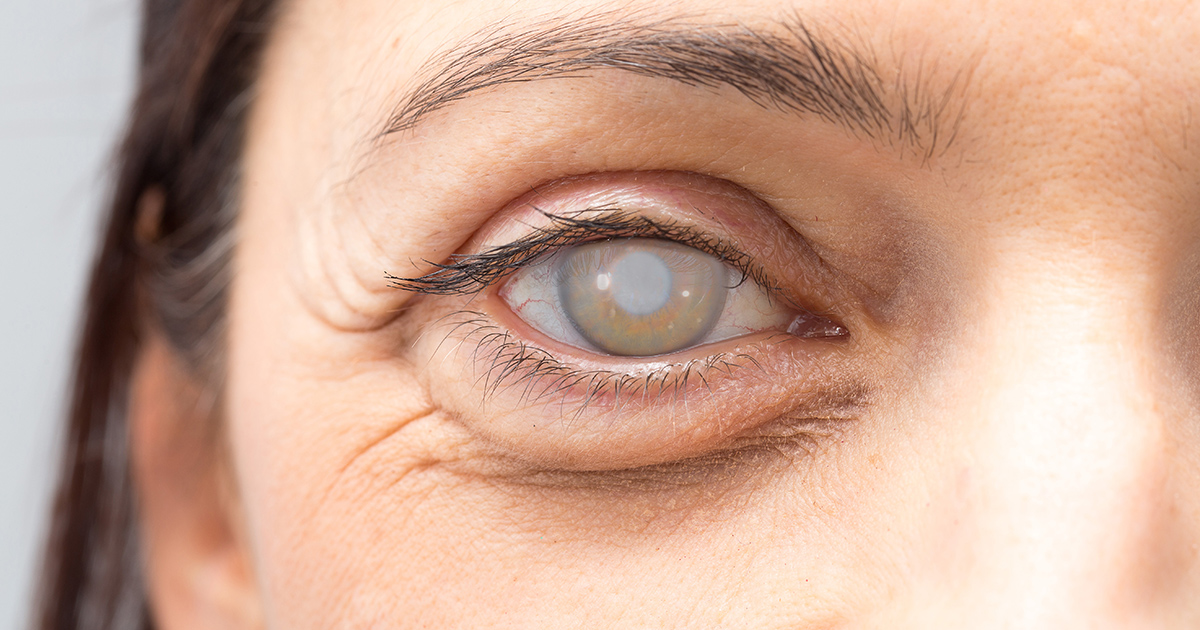
Corneal clouding is one of the most severe symptoms of trachoma, and it develops after years of repeated infection. Patients diagnosed with corneal clouding are typically referred for surgery since this symptom affects vision and can lead to blindness. For some patients, a corneal transplant procedure may be available to improve vision. Most often, doctors choose to start with a surgical intervention known as eyelid rotation surgery or bilamellar tarsal rotation. During this procedure, the specialist will make an incision in each of the upper eyelids, rotating the eyelashes and eyelid away from the cornea and back to a more normal position. This operation is performed under general anesthesia, and it can help limit the amount of corneal scarring and clouding that develops and prevent additional vision loss.