How To Treat A C. Difficile Infection
An infection that develops in the gastrointestinal tract caused by the Clostridium difficile bacterium is referred to as a C. difficile infection. Most individuals develop this type of infection because they have taken antibiotic medications to treat an unrelated infection that has thrown their gut microflora out of balance and allowed for the overgrowth of the Clostridium difficile bacterium. The C. difficile bacteria overgrowth in an individual's intestines produces symptoms associated with inflammation in the affected tissues due to toxins produced by the bacteria. Symptoms include fatigue, abdominal discomfort, nausea, fever, diarrhea, and dehydration. In a small number of cases, the C. difficile infection can affect an individual's entire body when it becomes progressively severe. While such cases require the use of aggressive treatment methods, C. difficile infections that are caught early can be treated with several less extreme methods. Learn about treatments for a C. difficile infection now.
Course Of Antibiotics

An individual affected by a C. difficile infection may need to take a course of antibiotics as the first part of their treatment. Antibiotics are a family of medications known to stop the growth or destroy certain bacterial microorganisms that cause illness and infection in humans and animals. Certain antibiotics that can kill off harmful bacteria can also kill off the good bacteria in an individual's gut that prevent bacterial overgrowth infections like C. difficile. While an antibiotic an individual is taking for another infection in the body can actually trigger their C. difficile infection, they still may need to take yet another course of a different antibiotic that will stop the C. difficile bacteria from growing any further. Antibiotics known to help patients with C. difficile infections include vancomycin, fidaxomicin, and metronidazole. An individual may experience a reoccurrence of their C. difficile infection if they take antibiotics to treat a different condition even while they are on antibiotics to treat their C. difficile infection.
Read more about the options for treating a C. difficile infection now.
Surgical Intervention

Surgical intervention is often reserved for individuals who have severe, unresolved, and non-responsive C. difficile infections. Severe C. difficile infections can cause patients to develop a condition referred to as toxic megacolon, which is when an individual's colon becomes abnormally wide within a time frame of several days because of the inflammatory process that has been triggered by their infection. When the colon dilates, expands, and distends to such a degree, it is unable to remove feces or gas from the body and can burst open. Surgery to remove all or part of the individual's colon, called a colectomy, may be required to eliminate the diseased tissues. The patients who require complete colon removal will also require an ileostomy so their body can still effectively eliminate waste. An ileostomy is a procedure where part of the individual's small intestine is pulled through an opening in their lower abdomen. Waste is then eliminated through a stoma or surgical wound opening into a disposable bag.
Continue reading to learn more about how to treat a C. difficile infection now.
Probiotics

Patients affected by a C. difficile infection may need to take probiotics as part of their treatment plan. Probiotics describe special supplements with live microorganisms within them, which serve the purpose of improving or maintaining an individual's normal microflora in their body. A C. difficile infection occurs when the microbes in an individual's gut become imbalanced or non-diversified, allowing the generally harmless C. difficile bacteria to grow dangerously out of control. While antibiotic mediation is used as the first method of treatment for C. difficile infections, it can be ineffective in individuals who have strains of the bacteria that are resistant to antibiotics. Probiotics may make antibiotics more effective in the treatment of C. difficile infections by competing with the bacteria for growth, by stimulating and modulating the immune system, by directly disrupting the metabolism of the C. difficile bacteria, and through improving general intestinal health. The most effective probiotics found to help fight C. difficile infections include Lactobacillus acidophilus, Bacillus probiotics, Saccharomyces boulardii, and Lactobacillus rhamnosus.
Uncover more C. difficile infection treatments now.
Fecal Microbiota Transplant

Individuals who have not been responsive to other forms of treatment for their C. difficile infection may need to undergo a fecal microbiota transplant. A fecal microbiota transplant is a procedure used to deliver healthy human donor stool to an individual who has a recurrent gastrointestinal infection that cannot be treated with antibiotics. Fecal microbiota transplant is performed with the use of a nasogastric tube or colonoscope to place the donor stool in the patient's colon. This type of transplant works to eliminate the C. difficile infection because certain microorganisms in the donor's healthy stool are infused into the colon of the patient. This process provides a new foundation for healthy bacteria to regrow in the colon that will stop the C. difficile bacteria from growing any further. Individuals who have C. difficile infections and undergo one or more fecal microbiota transplants have a success rate of over eighty-five percent. Donors for this procedure are always prescreened for the presence of medical conditions, infections in the blood, infections in the stool, viruses, parasites, and other potentially harmful or infectious bacteria.
Discover additional ways to treat C. difficile infections now.
Fluids And Nutrition
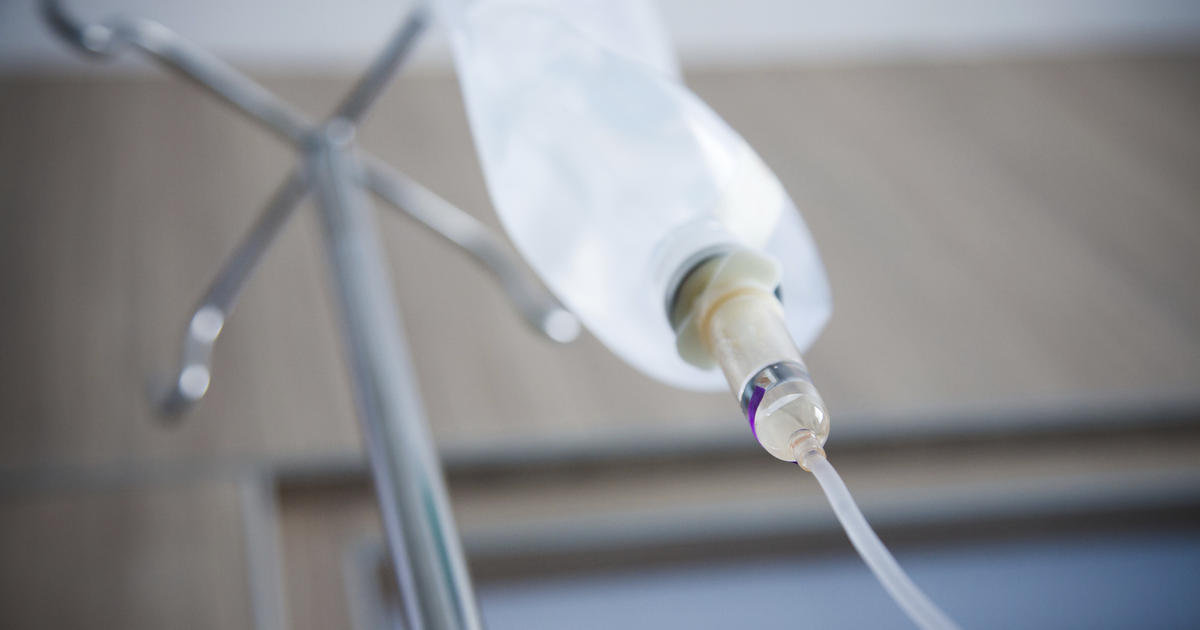
An individual who develops a moderate C. difficile infection may experience complications that result from the symptoms caused by the infection. When C. difficile bacteria grow out of control in the colon, it produces several toxins that cause widespread inflammation to the linings of the intestine. Damage and inflammation of the intestinal lining can impair the individual's ability to absorb nutrients and fluids from their digested food. The result of this malfunction is diarrhea because the stool contains extra fluid that should have been absorbed. Malnutrition can also occur from the inability to absorb important vitamins, minerals, and other substances from the digested food. Individuals who have diarrhea are likely to develop dehydration because they are losing a larger quantity of fluids from the body then the quantity they can take in. Dehydration should be treated in a hospital setting with supportive intravenous fluids when the patient is unable to keep fluids down. If a patient's condition reaches the point where they cannot keep food down and are in a febrile state, they may also require treatment with intravenous nutrition.