Treating And Managing Diabetic Macular Edema
Diabetic macular edema is an eye condition and complication of diabetic retinopathy that sometimes occurs in individuals with diabetes. In diabetic macular edema, fluid builds up in the macula as a result of untreated leaking blood vessels that develop from diabetic retinopathy. The macula is an area of the eye located at the center of the retina, and it controls the ability to see intricate details. Diabetic macular edema is more common in individuals who have had diabetes for many years and in patients who have high blood pressure and high cholesterol. Symptoms of diabetic macular edema include blurry vision, seeing floaters or spots in the visual field, and double vision. If left untreated, diabetic macular edema can cause blindness. The steps outlined below are helpful in treating diabetic macular edema.
Anti-VEGF Shots

Anti-vascular endothelial growth factor (anti-VEGF) drugs are used to stop the bleeding of leaking vessels and slow the growth of any abnormal blood vessels that may be present. These drugs are injected directly into the eye by ophthalmologists. Common types of anti-VEGF shots include bevacizumab, aflibercept, fluocinolone acetonide, and ranibizumab. Patients typically need to receive an injection at least once a month when first beginning this treatment. Before the injection is given, the doctor will numb the eye with anesthetic eye drops to prevent pain. Possible side effects from anti-VEGF medications include watery eyes, a burst blood vessel in the eye, swelling of the eyelids, seeing floaters in the visual field, and increased eye pressure. Patients should report any worrying side effects to their eye doctor, and they will have regular follow-up exams to monitor their vision.
Keep reading for more on treating diabetic macular edema now.
Macular Laser Surgery
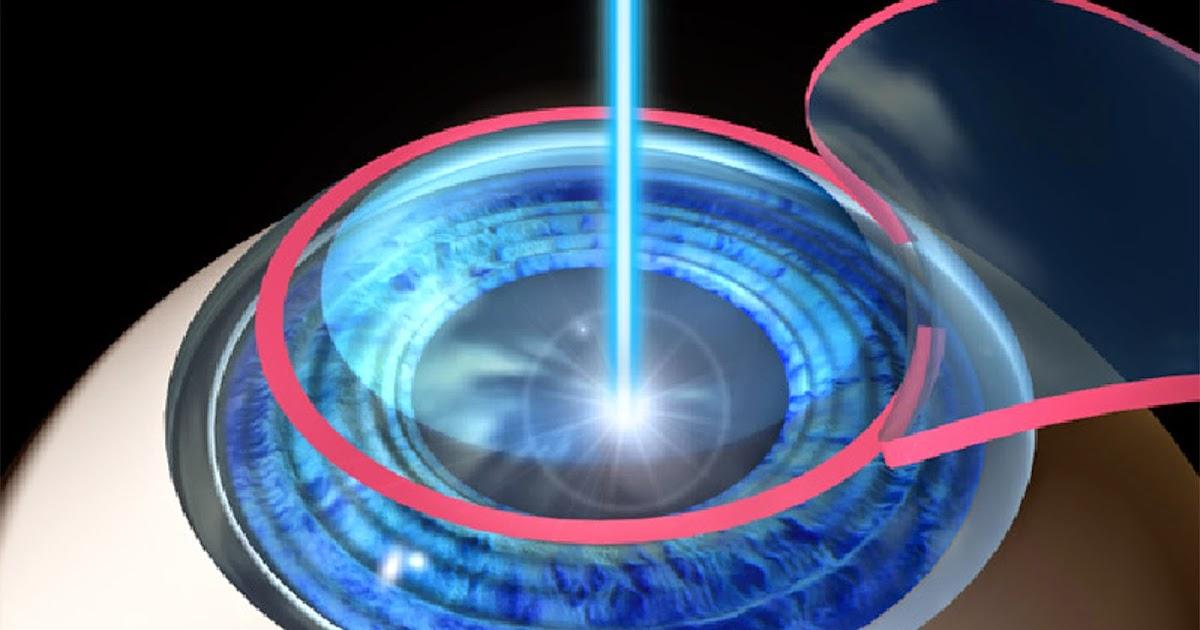
Various types of macular laser surgery may be used to help preserve remaining vision. In many cases, these operations may be able to improve vision too. One type of laser procedure is known as a focal laser, which is typically performed as an outpatient procedure at specialist eye clinics. Anesthetic drops are used to numb the eye before the treatment. In this painless procedure, a laser closes vessels in the macula to stop them from bleeding. The procedure can sometimes result in permanent empty areas in a patient's visual field, and it can take between three to six months after laser treatment for vision to completely recover. During this time, patients may be sensitive to light and can have irritation in the eye, including feeling as though something is stuck in the eye. During the recovery period, patients will be monitored closely with regular eye exams. If needed, laser surgery can be repeated.
Learn about the next method of treating diabetic macular edema now.
Corticosteroids
Corticosteroids are typically the first line of treatment for patients with diabetic macular edema caused by inflammatory diseases of the eye. These drugs are used to reduce inflammation in the eye, and they can be used as drops for the eyes or as oral tablets. Doctors can also inject them into the eye or the surrounding tissues of the eye. Three types of implants containing steroids are available for use. These provide an extended release of steroids and are placed directly into the eye by an ophthalmologist. To limit side effects, doctors try to use drops or other therapies that administer the steroids directly into the eye instead of oral tablets, as oral medication often has more severe side effects than other methods. Prednisolone acetate, difluprednate, fluorometholone, and loteprednol are some of the most commonly recommended steroid drops. Possible side effects of these drops include blurred vision, cataracts, increased eye pressure, and increased sensitivity to light. Patients may need to take several types of steroids as part of their treatment. Any unusual side effects should be reported to the ophthalmologist who recommended the medication.
Get to know more about how to manage diabetic macular edema now.
Eye Drops

Patients with diabetic macular edema frequently need to use prescription drops for their eyes at home. Depending on their condition's severity, some patients may need to use three to five different types of drops each day. Typically, drops are used in the morning and evening, but some medications may need to be administered three times per day. The most commonly used drops include antibiotics to prevent infection and steroids to reduce inflammation. Patients may also need to use special drops that can lower the pressure in their eyes. When using eye drops, patients may experience temporary burning immediately after placing the drop in their eye, and they may also have blurred vision. Typically, patients will need to continue using drops for several weeks or months, especially if they are recovering from recent eye surgery. Some of the most common drops include beta blockers, prostaglandins, and moxifloxacin (an antibiotic). While using drops, patients will have routine follow-up appointments. A variety of drops are available, and patients should ask their eye doctors about switching to a different drop if they experience bothersome side effects.
Learn more about treating diabetic macular edema effectively now.
Managing Blood Sugar And Blood Pressure

Managing blood sugar and blood pressure may help diabetes patients reduce the risk of developing diabetic macular edema. Patients should aim to adopt a healthy lifestyle to help with this. Fast food, processed food, and saturated fat should be limited, and patients should try to include higher amounts of whole grains, fruits, and vegetables in their diets. Online apps for food logging can help patients become more mindful of their dietary choices, and patients may also wish to consider having a consultation with a nutritionist who specializes in diabetes management.
Doctors recommend patients monitor their blood sugar regularly, and patients can ask for more comfortable blood glucose testing devices if they find glucose tests particularly painful. High blood pressure can make diabetes worse, and doctors frequently suggest patients monitor their blood pressure at home. Patients can purchase automatic blood pressure monitors designed for home use, and some of these will connect to smartphone apps to log measurements automatically. Patients should take blood pressure readings while they are at rest. Measurements taken at home can be compared with readings taken at the doctor's office, and medication to reduce blood pressure may be recommended if readings are consistently high.