Treatment Options For Keratoconus
Keratoconus usually starts during the teenage years or as a young adult. The progressive eye disease, which can affect one or both eyes, usually presents itself with symptoms including blurred or distorted vision, increased sensitivity to bright light, a need for frequent changes to prescription glasses, and worsening or clouding of vision. The rapid advancement in medicine made treatment options for this disease not only widely available but also cost-efficient. Treatment options depend on the severity of a patient's keratoconus. This article will focus on the most preferred options for treating keratoconus.
Specialized Contact Lenses

Patients diagnosed with keratoconus will typically end up wearing specialized contact lenses that vary depending on their condition's severity. Soft contact lenses are mostly recommended for individuals diagnosed with an early stage of keratoconus. Scleral lenses, hybrid lenses, or piggyback lenses are prescribed to patients diagnosed with advanced keratoconus. Patients with very irregular shape changes in their cornea use scleral lenses, which are designed to sit on the white part of the eye in order not to touch the cornea. They are also larger compared to gas permeable lenses. Scleral lenses are made in such a way to cover even relatively large areas of the distorted cornea. Hybrid lenses feature a rigid center with a soft outer ring and are prescribed to patients who cannot wear hard contact lenses, as are piggyback lenses.
Continue reading to reveal more ways to treat keratoconus now.
Corneal Transplant

A corneal transplant is advised to patients who have corneal scarring or thinning. A research study from the Netherlands found transplantation led to improved vision and stabilization of the disease in most of their participants. It also determined that placing the donor tissue in the middle of the cornea helps in faster healing period.
There are also several kinds of corneal transplant surgery recommended for patients suffering from keratoconus, such as lamellar keratoplasty. This is a partial-thickness procedure in which only a section of the cornea is replaced. Penetrating keratoplasty is a full transplant and removes the full thickness of the cornea and replaces it with donor tissue. Lastly, deep anterior lamellar keratoplasty involves preserving the endothelium of the cornea and is useful for a successful transplant, as the surgery helps avoid transplant rejection by preserving a critical inside lining in the cornea.
Understand more about treatment options for keratoconus now.
Topography-Guided Conductive Keratoplasty
Topography-guided conductive keratoplasty is for patients looking for an effective and non-invasive procedure. It makes use of radiofrequency to correct presbyopia and hyperopia with or without astigmatism. This treatment is also cost-effective, making it an important achievement in refractive surgery. Conductive keratoplasty is dependent on the impact of temperature on the cornea’s biomechanical properties. The collagen of the cornea dehydrates and retracts at a certain temperature but can maintain its original configuration upon cooling. Patients who underwent this procedure were found to have achieved 20/40 vision. Foreign body sensation and light sensitivity are the most common side effects of this surgery. Aside from these two, some patients also complained of astigmatism, which is usually caused by inaccurate cornea markings, asymmetric application of spots, and more than one insertion of the probe on the same spot.
Learn more about how to treat keratoconus now.
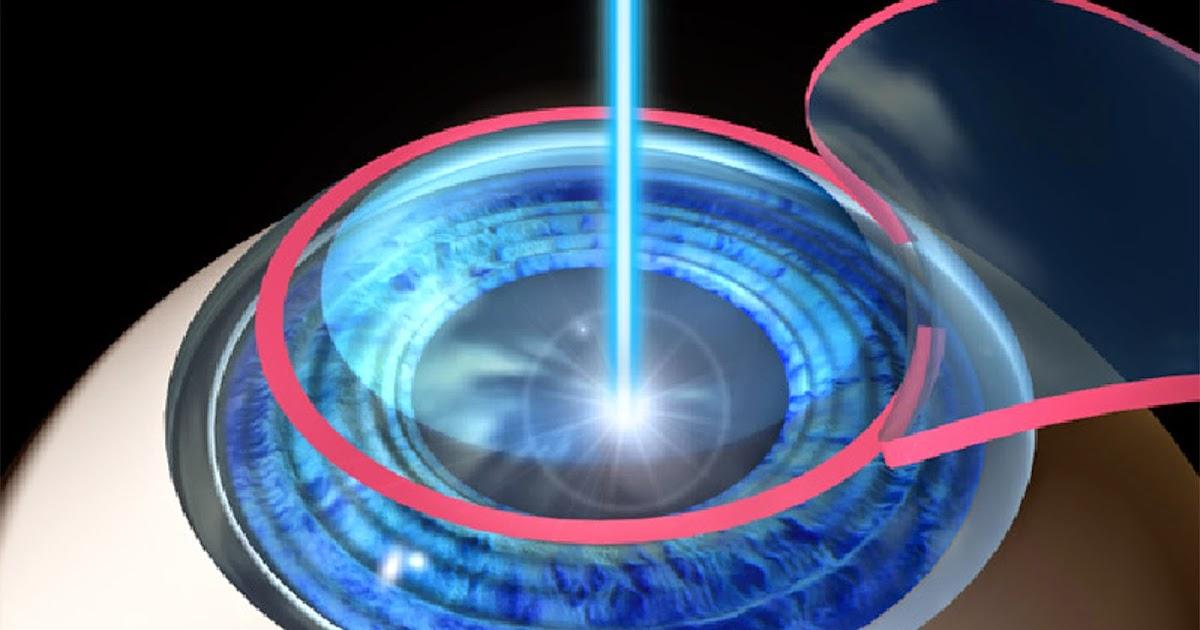
Corneal Crosslinking

Corneal crosslinking is a procedure approved by the Food and Drug Administration for keratoconus in 2016. The procedure makes use of special eye drop and ultraviolet-A light to correct irregularities in the cornea, which helps make the cornea thicker. There are various techniques of doing this procedure. The Epithelium-off technique involves removing the epithelium before administering the special eye drop. Researchers claim this method allows better absorption of vitamins and light into the eye. The second method is when the eye drop is administered without taking off the epithelium. This type is also painless and entails a shorter recovery period. The procedure is usually done at a health facility. The physician starts the procedure by administering a drop to numb the corea and calm the patient down. They then drop vitamin B12 or riboflavin into the patient's cornea. The rest of the procedure entails lying down and looking into the light. The procedure usually lasts thirty minutes to an hour.
Get the details on the next way of treating keratoconus now.
Do Not Rub Eyes

The American Academy of Ophthalmology claims constant hard rubbing of the eyes can cause keratoconus. The organization explained there is an increased risk factor for this, especially among teenagers and young adults. It added individuals diagnosed with connective tissue disorders like osteogenesis imperfectashould refrain from constantly rubbing their eyes as it could lead to thinning cornea tissue. An immediate visit to a physician is recommended for individuals who feel the constant need to rub their eyes. It is especially advised for individuals suffering from atopic or allergic conjunctivitis. A visit to an ophthalmologist, not eye rubbing, is the best way to check whether keratoconus or another eye issue is present.