10 Facts You Need To Know About Ulcerative Colitis
Ulcerative colitis (UC) is a form of inflammatory bowel disease (IBD) that impacts the digestive system by causing inflammation, ulcers, and sores in the inner lining of the large intestine (colon) and rectum. Ulcerative colitis symptoms can be mild, moderate, or severe, at times potentially causing life-threatening complications. There is still much to learn about this condition. With more knowledge about ulcerative colitis, individuals with the disease, family members of those affected by it, and medical professionals can have a better understanding of how to manage and control the condition.
Cause Of Ulcerative Colitis

Despite many research studies and test trials, the cause of ulcerative colitis is not known. In the past, it has been suspected that stress and diet may have caused the condition. However, there is not enough research to back these claims. It is now thought that diet and stress can aggravate ulcerative colitis but they are not the cause. A possible cause of the disease is an abnormal immune system response. This may occur when the immune system acts to combat an invading bacterium or virus and instead the immune system attacks the cells of the gastrointestinal tract as well. Another cause may be genetics, as ulcerative colitis tends to be more prevalent amongst individuals who already have a family member with the disease.
Symptoms

The symptoms of ulcerative colitis, also known as flare-ups, depend on the location and the severity of the inflammation. Symptoms include rectal bleeding and stools with blood, abdominal pain and discomfort, diarrhea with mucus or blood, reduced appetite, nausea, an urgency to defecate, constipation, rectal pain, and tenesmus which is the inability to move bowels despite urgency. There are symptoms that are outside the digestive system such as frequent fevers, skin sores and rash, fatigue, weight loss, anemia, and joint pain. Some factors that can trigger the symptoms of UC are taking nonsteroidal anti-inflammatory drugs (NSAIDs) such as naproxen, aspirin, and ibuprofen; use of antibiotics; missing doses or wrong doses of medication; smoking; eating foods that can aggravate the digestive tract; and stress.
Types Of Ulcerative Colitis
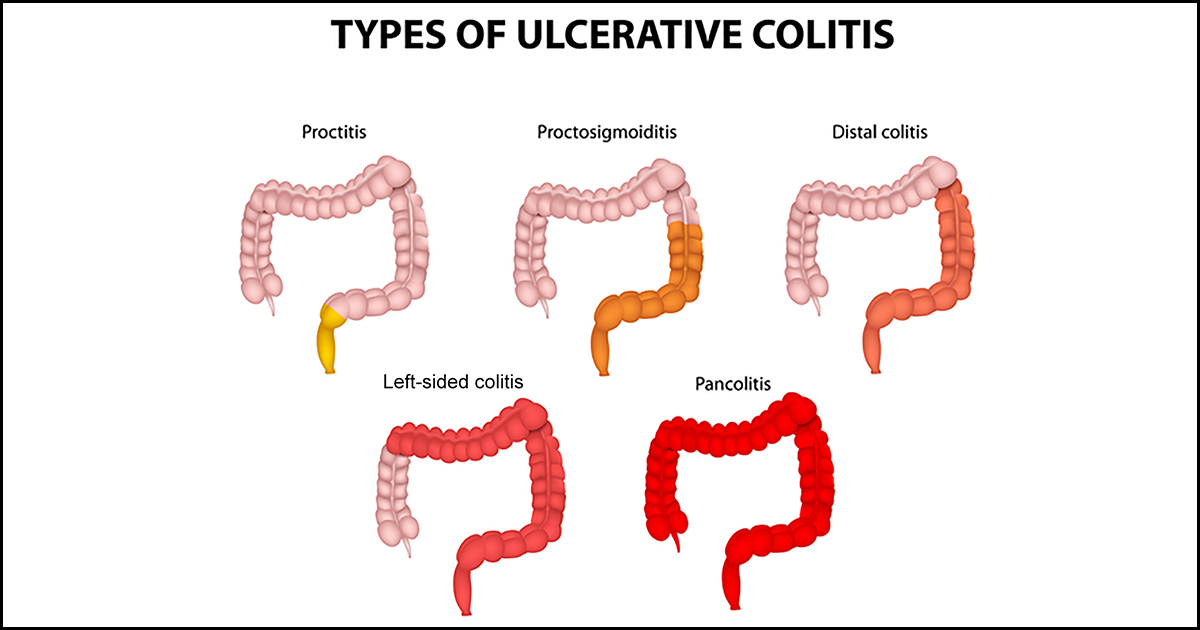
There are various types of ulcerative colitis based on the location of the inflammation in the colon. Pancolitis or pan-ulcerative colitis usually affects the whole large intestine and results in bloody diarrhea that can be severe, abdominal pain, evident weight loss, and fatigue. With ulcerative proctitis, the inflammation is often located in the area close to the anus and rectum. Rectal pain, bleeding, and a feeling of urgency are the main sign of proctitis and it is considered to be the mildest type of ulcerative colitis. Proctosigmoiditis includes the rectum and sigmoid colon, which is the lower part of the large intestine. Signs of proctosigmoiditis include abdominal pain and cramps, tenesmus which is a sudden and frequent need to move bowels, and fatigue. Left-sided colitis involves the rectum up to the sigmoid and the descending colon. Symptoms are significant weight loss, pain and cramping on the left side of the abdominal, and bloody diarrhea. An uncommon type is acute severe ulcerative colitis which impacts the whole colon and induces fever, loss of appetite, severe pain, bleeding, and frequent diarrhea.
Complications Of Ulcerative Colitis

As ulcerative colitis progresses and if it remains severe, there are possible complications associated with the condition. Potential complications of the disease include osteoporosis (bone loss); severe bleeding; heightened risk of blood clots in arteries and veins; liver disease; perforated colon (hole in colon); severe dehydration; inflammation of eyes and skin; arthritis; toxic megacolon (frequent swelling of the colon); increased risk of colorectal cancer; primary sclerosing cholangitis (inflamed and/or damaged bile ducts). Some medications used to treat ulcerative colitis can cause some complications. For example, the prolonged use of corticosteroid medication which is used to treat UC can lead to osteoporosis and the weakening of the bones. In children and adolescents, failure to grow or poor growth and development can occur as a complication of ulcerative colitis.
Treatment

The treatment of ulcerative colitis is based on the severity and progression of the disease. The common components of treatment include medicine and diet changes. If an individual’s condition is considered severe, they may require more medication and potentially surgery. The goals of treatment for UC are controlling the inflammation, remission, and maintaining remission. Part of the treatment involves treating the symptoms of ulcerative colitis such as anemia, malnutrition, and inflammation outside the colon. Those that are in remission or showing no signs of the disease may not have to take medication. However, a physician may still require the use of medicine to maintain remission. At the present moment, there is no medical cure for ulcerative colitis.
Categories Of Medications For Ulcerative Colitis

There are several categories of medications for ulcerative colitis. Antibiotics including ciprofloxacin, metronidazole, and others can be used to treat infections or other complications of UC. Aminosalicylates (5-ASAs) reduce the inflammation in the large intestine and are taken to manage the remission of the disease. Corticosteroids (steroids) work by suppressing the immune system and decreasing inflammation in the inner lining of the digestive system. most times, steroids are not prescribed for prolonged use but instead for short-term control of symptoms and active disease. Immunomodulators (immune modifiers) also suppress the immune system to prevent inflammation. Biologics (biologic therapies) target a distinct pathway and suppresses the body’s immune response.
Treatment Based On Severity And Alternative Treatment

For mild symptoms of UC, steroid medicine, aminosalicylates, enemas or suppositories, antidiarrheal medication, and diet changes may be suggested. For moderate to severe symptoms of UC, higher doses of the previously mentioned medications may be prescribed, immunomodulator medicines or cyclosporine, biologics, surgery and the removal of the colon. In the hospital, to treat anemia, severe diarrhea, and nutrition deficiencies due to malabsorption of nutrients from foods, treatment may include blood transfusions, replacing electrolytes and fluids lost. There are also natural or alternative medicine treatments and therapies available in place of prescribed medications. These therapies may include nutritional supplements, herbal remedies, acupuncture, and diet changes. It is recommended that anyone considering alternative treatments have a discussion with their doctor.
Eating With Ulcerative Colitis

There are some diets that are advised for UC including the low-residue diet and specific carbohydrate diet. A low-residue diet consists of low-fiber foods and decreasing the consumption of high-fiber foods. The specific carbohydrate diet is a low-carbohydrate diet which recommends the intake of certain carbohydrates that are easy to digest. Suggested foods for UC include avocados, plain yogurt and probiotic-rich foods, nut butters, lean poultry and meats, fruits, fish, grains, eggs, cooked vegetables, unsweetened canned fruits, chicken broth, white rice with turmeric, unsweetened applesauce, and squash. Recommended drinks for those with UC include water, low-sugar sports drinks and fruit juice, herbal and decaffeinated teas like chamomile tea, peppermint tea, decaffeinated green teas, smoothies, and nondairy kinds of milk like almond milk.
Foods to Avoid For Those With Ulcerative Colitis

There are some foods that are taught to worsen and aggravate the symptoms of ulcerative colitis. For UC sufferers the following foods are recommended to avoid, especially during a flare-up: dairy products; foods containing sulfur or sulfate; raw fruits and vegetables; peas, dried beans, and legumes; foods high in fiber; fatty meats; popcorn; sugar-free gum and candies; nuts and seeds; gluten; refined sugar; spicy foods. Drinks to avoid include coffee, any caffeinated drink, milk, carbonated beverages and sodas, and sugary juices.
Ulcerative Colitis Vs. Crohn’s Disease
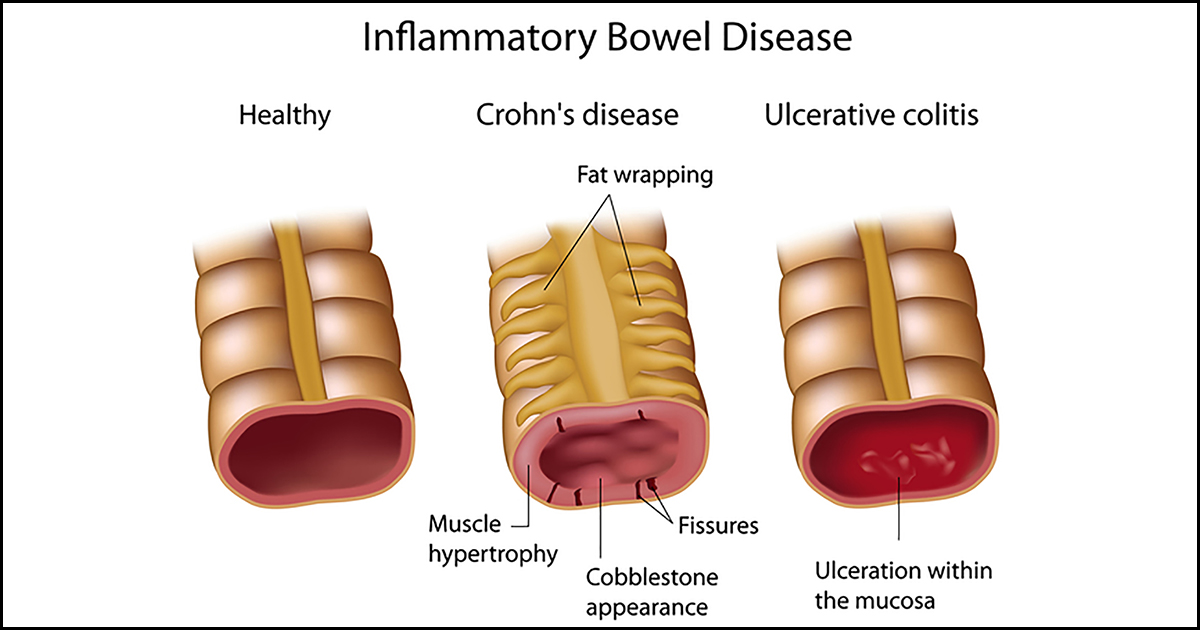
Ulcerative colitis and Crohn’s disease are both inflammatory bowel diseases. Both conditions involve long-term inflammation in the digestive system. With UC, the inflammation only affects the inner lining of the large intestine and rectum. However, in Crohn’s disease, the inflammation can impact the entire gastrointestinal tract. There are similar symptoms of the diseases including constipation, diarrhea, abdominal pain, rectal bleeding, an urgency to defecate, weight loss, fatigue, and low appetite. The main differences of the conditions are location, where the inflammation is, and specific symptoms. For example, blood in stools is a symptom that is more common with UC compared to Crohn’s. In addition, Crohn’s can have more symptoms that involve other parts of the body such as anal fissures, mouth sores, and other infections.