Common Causes And Risk Factors For Peritonitis
Peritonitis is a condition in which the peritoneum, a membrane that covers the abdominal wall and the organs within the abdomen itself, becomes inflamed. Symptoms generally include fever, nausea, abdominal pain, thirst, constipation, and bloating. Patients may also experience decreased urine output, loss of appetite, and diarrhea. Peritonitis requires urgent medical attention to prevent the spread of the infection; if left untreated, it can be life-threatening. To diagnose this condition, doctors may perform x-rays, ultrasounds, or CT scans to check for perforations in the abdominal area. A sample of fluid from the peritoneum may be obtained and cultured to check for bacteria. Treatment options include antibiotics, pain medications, intravenous fluids, and surgery.
Some of the most common causes and risk factors for peritonitis are discussed below.
Pancreatitis
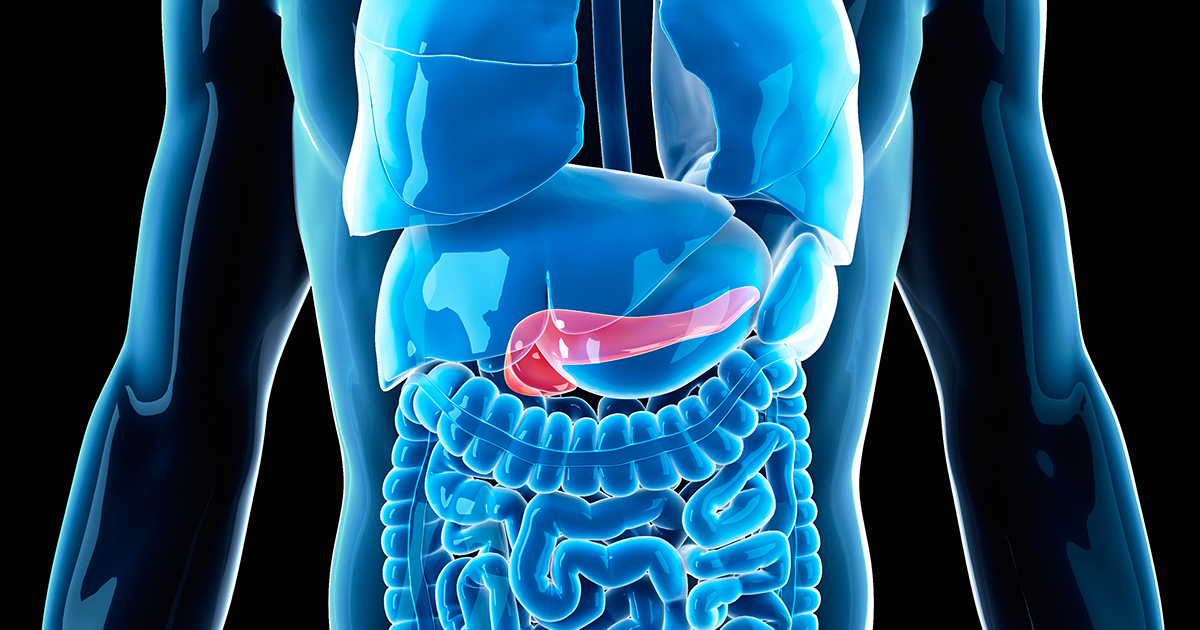
Pancreatitis is an inflammation of the pancreas, and it is normally caused by an infection, gallstones, or significant alcohol consumption. If the infection spreads beyond the pancreas, peritonitis may develop. Patients with pancreatitis may have an elevated heart rate and upper abdominal pain, and fever, nausea, back pain, and abdominal swelling may also be present. Blood tests, glucose tolerance tests, imaging studies, and a biopsy of the pancreas may all be needed to confirm a diagnosis of pancreatitis. Treatment of pancreatitis is provided in the hospital, and patients will have their heart, lung, and kidney function closely monitored since pancreatitis can cause damage to these areas. Some patients with severe pancreatitis may need to be treated in the intensive care unit. Surgery to remove gallstones or the gallbladder can sometimes resolve pancreatitis, and patients may be advised to eat a low-fat diet following the surgery.
Get the details on more causes and risk factors of peritonitis now.
Injury Or Trauma
Injury or trauma to the abdomen, including injuries from car accidents, contact sports, and falls, may result in peritonitis. In this case, a blow to the abdomen ruptures the abdominal wall, allowing bacteria and substances from other parts of the body to enter the abdomen. Patients who injure their abdomen should watch for fever, nausea, or pain, and they should seek prompt medical attention to reduce the risk of peritonitis. If patients develop abdominal pain that is so severe they cannot sit or find a comfortable position, they should seek emergency medical care. X-rays, CT scans, ultrasounds, and physical examination can all be used to assess trauma. If doctors suspect peritonitis, they will begin immediate treatment with intravenous fluids, and antibiotics will also be given to reduce the risk of life-threatening sepsis, a potential complication of peritonitis. Patients who have had an injury or trauma will be monitored several times an hour by hospital staff, and they will have their blood pressure, pulse, respiration rate, and temperature measured regularly. In particular, patients should alert their medical team if they develop any abdominal swelling, nausea, bloating, constipation, or diarrhea.
Learn more about risk factors and causes of peritonitis now.
Ruptured Appendix

A ruptured appendix is one of the major causes of peritonitis. The rupture of the appendix creates a hole in the gastrointestinal tract, providing a potential point where dangerous bacteria can enter the peritoneum and spread throughout the abdomen. A ruptured appendix is considered a medical emergency, and immediate surgery is performed to remove the appendix and clean out the abdominal cavity. An appendix may rupture after an episode of appendicitis, an inflammation of the appendix. Patients with appendicitis often experience sudden pain in the right lower section of the abdomen, and this pain may increase when the patient coughs or walks. Bloating, nausea, diarrhea, constipation, and low-grade fever may occur too. Patients with appendicitis are normally treated in the emergency room, and immediate surgery is generally recommended to remove the appendix and prevent a rupture. While in the emergency room before surgery, patients with appendicitis are closely monitored for any signs of rupture.
Continue reading to reveal more peritonitis risk factors and causes now.
Peritoneal Dialysis

Peritoneal dialysis is a significant risk factor for the development of peritonitis. Unlike other methods of dialysis performed through a machine outside of the body, peritoneal dialysis uses the peritoneum to take over some of the filtration normally done by healthy kidneys. Peritoneal dialysis is typically done in the patient's home, and it involves using a catheter to fill the peritoneum with dialysate, a cleaning solution. After a specified period, the patient drains the dialysate from the peritoneum and refills the area with a fresh dialysate solution. The drainage and refill process is known as an exchange, and each exchange normally takes thirty to forty minutes. Patients may need to do several exchanges each day. To reduce the risk of peritonitis while undergoing peritoneal dialysis, patients should ensure the place they perform their dialysis is clean, dry, and free of both plants and pets. When handling catheters and other dialysis equipment, patients should ensure their hands are clean, and they may need to wear a face mask during their exchanges. The area around the catheter should be cleaned daily with an antiseptic, and patients should watch for fevers, nausea, or any other symptoms that could indicate possible peritonitis.
Uncover more information regarding the risk factors and causes of peritonitis now.
Diverticulitis

Diverticulitis is a condition in which the tiny pouches along the intestinal wall become infected. If one of the infected pouches ruptures, this could leak intestinal waste into the peritoneum, leading to peritonitis. Diverticulitis can cause severe abdominal pain, fever, and cramping on the left side of the abdomen. Patients may also have bright red blood in their stools. Doctors normally use a colonoscopy to diagnose diverticulitis, and patients who have severe cases will be given intravenous antibiotics in the hospital. To give the colon time to rest, they will also be fed through a feeding tube. Patients who have abscesses as a result of their diverticulitis may need surgery to drain these, and a temporary colostomy may be recommended to help the intestines heal.