Guide To Diagnosing And Treating Atelectasis
If the small sacs in the lungs deflate or become filled with fluid, this is often referred to as atelectasis, more commonly referred to as a collapsed lung. This collapse of the lung can affect the entire lung, as in a full collapse, or may only affect a portion of the lung, which is considered a partial collapse. Atelectasis is more likely to occur following a surgical procedure because of anesthesia complications, but this condition may also occur as a complication of another lung disease or infection or as a result of the inhalation of a foreign object into the lung. A medical professional must diagnose this condition to provide the appropriate treatment that will restore lung function.
Get the full details on diagnosing and treating atelectasis now.
Thorax Ultrasound

In the past, there were very few ways to tell if a patient had a collapsed lung, and of these, most were fairly invasive and often resulted in serious complications or death to the patient. Today, a thorax ultrasound chest can provide a valuable image to medical professionals and is performed in a noninvasive manner. Sounds waves inaudible to the human ear move at different speeds depending on the type of tissue, producing an image that can differentiate between bones, soft tissues, and air. With a thorax ultrasound, the examining physician can then make a proper diagnosis, such as for atelectasis.
Keep reading for details on how a bronchoscopy can help in diagnosing atelectasis next.
Bronchoscopy

Sometimes the results offered by a thoracic ultrasound are not conclusive. In these cases, the physician may want to take a much closer look with a bronchoscopy. During this procedure, the patient's physician will send a tube down into their airways, either through the nose or mouth, to see the airways and lungs more closely. If a patient inhaled a foreign object, the physician might be able to remove it during this procedure. Although the procedure itself generally takes an hour or less, the entire process, including preparation and recovery times, may last for four hours or more. Additionally, there are slight risks of complications, including fever, bleeding, and a collapsed lung.
Learn more about diagnosing atelectasis now.
Oximetry

Oximetry is a test that might be used to help determine how severe atelectasis is. It's a simple and painless test that measures the amount of oxygen in the patient's blood. A device similar to a clip is placed on a certain body part. In most cases, doctors or nurses will place it on the patient's finger, but their ear lobes might also be used. The probe measures the amount of oxygen in the patient's blood by using light. The information gathered allows a healthcare provider to determine whether the patient needs extra oxygen or not. Oximetry may be used after the doctor has made an atelectasis diagnosis using a simple examination and chest X-ray.
Uncover more on how to accurately diagnose atelectasis now.
CT Scan

A computerized tomography (CT) scan uses more sensitive techniques than X-rays. When a chest X-ray isn't providing enough information, doctors will sometimes use a CT scan to determine the type and cause of atelectasis. With this type of scan, a machine gathers a series of X-rays taken at multiple angles surrounding the patient's body. Using computer software, the machine creates cross-section images of the patient's bones, lungs, blood vessels, and other tissues. Unlike X-rays, which only provide one image and angle, CT scans create more detailed and layered images. CT scans are used to visualize almost all areas of the body, and they tend to be relatively quick procedures.
Continue to discover how to treat atelectasis now.
Tumor Shrinkage And Removal
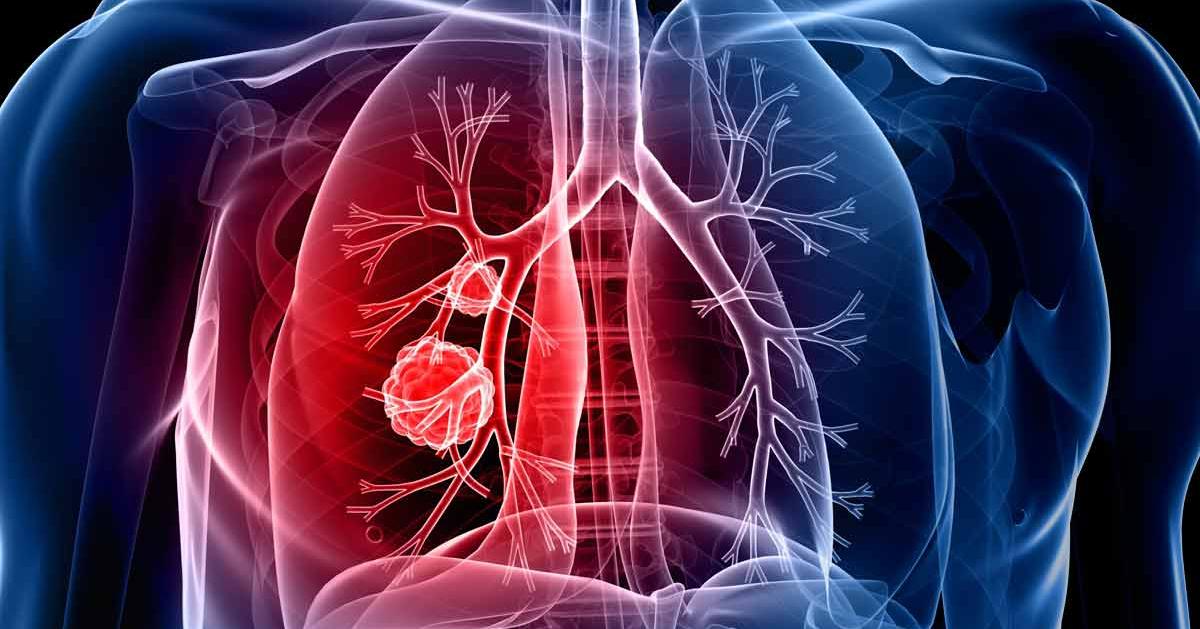
If there is a tumor keeping a portion of the sacs within the lungs from inflating properly, tumor shrinkage and removal could be a priority to address a collapsed lung. Medications may be used to help shrink the tumor, or it may be removed through a surgical procedure. If the tumor is small enough, the surgeon may be able to remove it during a scope procedure used to diagnose the reason for atelectasis. For larger tumors, physicians may recommend radiation or chemotherapy instead of surgery or before or after a surgical procedure is performed.
Learn more about treating atelectasis now.
Continuous Positive Airway Pressure

Continuous positive airway pressure, more commonly referred to as CPAP, has been shown to be beneficial for patients with atelectasis. A mask is placed over the patient's nose or the patient's mouth and nose. A machine pumps gas mixed with the appropriate amount of oxygen into the patient's lungs in a manner that mimics regular breathing patterns. CPAP can be beneficial to patients unable to cough firmly enough and whose oxygen levels are low due to the collapse of the lung. It is not only effective at treating cases of atelectasis, but is often used after certain types of surgery as a way to reduce the risk of developing collapsed lung following surgery.
Get to know the next method of treating atelectasis now.
Chest Physiotherapy

If there is an obstruction in the airways due to mucus or if there is a collection of fluid in the pleural region, it might be necessary for a physical therapist or a respiratory therapist to use vigorous chest physiotherapy. This treatment technique is most commonly used on patients with cystic fibrosis, though it is also very effective at helping to expand the lungs to help with sac inflation. For this treatment, the therapist will use percussion, which is basically a clapping on the ribs around the lungs to create vibrations. The vibrations help move mucus or other fluids to be expelled from the lungs, creating more room for air in the airways.
Continue to reveal more options for treating atelectasis now.
Deep Breathing Exercises

After atelectasis patients have surgery to re-expand a portion of collapsed lung tissue, it's important to use certain chest physiotherapy techniques to breathe deeply. It's also best to learn the techniques prior to surgery. Deep breathing exercises are one portion of chest physiotherapy, while other devices can help with deep coughing. Doing these exercises helps increase the patient's overall lung volume and remove secretions within the lungs. Breathing deeply moves air to the bottom of the lungs rather than just the top of the chest. It also increases the patient's oxygen intake and helps the supply of oxygen in their blood. To engage in deep breathing exercises, patients should get in a comfortable position lying down or sitting up. They should then put their hands over their stomach, breathe in deeply through their nose, and keep breathing until their lungs feel filled with air. Then, patients must purse their lips and slowly blow out, concentrating on making their stomach muscles sink. They should repeat this for several breathing cycles.
Learn about another method of treating atelectasis now.
Postural Drainage

Postural drainage is a way of draining the airway to help clear mucus and other secretions from the lungs. While the technique is most commonly used for chronic obstructive pulmonary disease patients, it can also be used for atelectasis. The lungs have five lobes, with two on the left and three on the right portion of the chest, and every lobe has further segments. The postural drainage goal is to drain the mucus out of the lobes and into the larger airways, so patients can more easily cough it up. To engage in postural drainage, patients will use a combination of clapping on their chest with cupped hands and vibrating their chest with their hands held flat.
Get more details on how to treat atelectasis now.
Medication

In cases where the condition leads to serious pleuritic pain, doctors might prescribe opioids on a temporary basis to help relieve pain. While taking opioids, patients should engage in deep breathing exercises and consciously cough to bring up phlegm and increase their oxygen circulation levels. After an operation to reinflate tissue, doctors might use an intercostal nerve-blocking medication or epidural analgesia to relieve pain without leading to a decrease in respiration. Doctors may also prescribe medications to help thin mucus and loosen it. Combined with postural drainage techniques, these medications can make it much easier to remove mucus from the respiratory system.