A Comprehensive Guide To Duane Syndrome
Duane syndrome is a rare eye movement disorder often classified as a type of strabismus, in which eye movements are restricted based on the case’s severity and type. It is present at birth, although it may not be detected immediately. This condition prevents the eye from moving outward towards the eye, inward towards the nose, or even both. When the eye moves inward, the eyelid will close partially,Âand the eyeball will retract into the socket.
Although Duane syndrome is a rare condition, it is still essential to understand the signs and symptoms, causes, the difference between the three major types, and how to treat this disorder. Start reading and dive into all of these details now!
What Causes Duane Syndrome?

Duane syndrome is the result of improperly developed nerves, specifically the sixth and third cranial nerves, to the eyes muscles. The sixth cranial nerve is what controls the lateral rectus muscle, which is in charge of moving the eye outward. The third cranial nerve controls the medial rectus muscle, which pulls the eye inward. Patients with Duane syndrome may also not have a sixth cranial nerve at all.
Unfortunately, the reason these nerves do not develop properly is unclear, though research is currentlyÂbeing conducted. Some research indicates Duane syndrome may be the result of several genetic or environmental factors, such as genetic mutations, which compromises embryonic development. The cranial nerves and eye muscles typically develop between the third and eighth week of a woman’s pregnancy, and as such, this is when the factors compromising development would occur. Duane syndrome appears more often in girls than boys, though it is also unclear as to why this is the case.
Continue reading to learn about the three major types of Duane syndrome and their characteristics.
Types Of Duane Syndrome And Characteristics

How Duane syndrome presents itself depends on the type the individual has. Typically only one eye is affected, though it is possible for both to be compromised.
Type 1, the most common, is characterized by the affected eye’s limited ability to move outwards towards the individual’s ear. The eye’s ability to move inwards is either entirely normal or close to it. In Type 1, the affected eye opening will narrow,Âand the eyeball will pull in when the patient looks inward. The reverse of this occurs when looking outward. Type 2, the rarest, is characterized by the affected eye’s limited ability to move inwards towards the nose and the usual ability to move outwards. In this type, the eye-opening will narrow,Âand the eyeball will pull in when the patient looks towards the nose. The affected eye in Type 3 has a limited ability to move both outwards and inwards. Like the other types, in Type 3 the eye-opening will narrow,Âand the eyeball will pull in when the patient looks inward.
Continue reading to learn about the subtypes of Duane syndrome and how they present themselves.
Subtypes Of Duane Syndrome

Although there are just three major types of Duane syndrome, this condition can be further broken down into subtypes, based on how the eyes look when the patient looks straight. As previously mentioned, Duane syndrome affects just one eye more often than it does both. Based on this information, the left eye is the affected eye more often than the right, although researchers are unsure as to why this is the case. Thus, the left eye is most often what differentiates the subtypes.
Subtype A occurs when the patient’s affected eye is turned inwards, called esotropia. In subtype B, the affected eye is turned outwards, called exotropia. The final subtype, subtype C, occurs when the patient’s eyes are in a straight position.
Continue reading for information on additional symptoms and indicators of Duane syndrome.
Additional Symptoms And Indicators
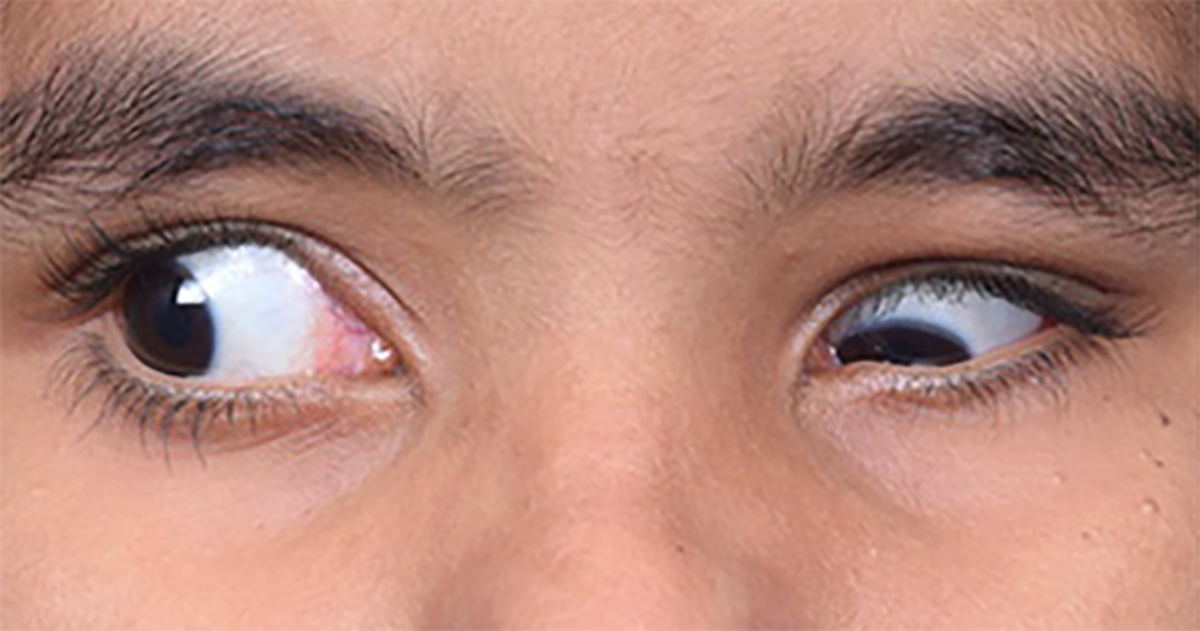
Other indicators a patient may have Duane syndrome include an abnormal head positioning, upshoot or downshoot, and the briefly mentioned narrowing of the eyelid. Abnormal head positioning can mean the patient maintains an abnormal head posture to keep their eyes straight or they turn their head to do that. Upshoot or downshoot implies with specific eye movements, the patient’s eye may periodically stray upward or downward. Eyelid narrowing in Duane syndrome means the affected eye is likely to appear smaller than the unaffected eye.
Although most individuals with Duane syndrome will not have other eye issues, it is possible for patients to develop amblyopia, an eye condition causing vision loss in the affected eye. For full details about amblyopia, check out Amblyopia (Lazy Eye); Symptoms, Causes, And Treatment. This typically occurs if the head position is unable to make up for the weak nerves and muscles, causing constant misalignment. Along with rarely developing other eyes issues, most patients do not develop other health issues. However, some problems found in rare cases include hearing loss, skeletal malformations, kidney problems, and nervous system disorders. Specific syndromes patients may develop in rare cases include Goldenhar syndrome, Holt-Oram syndrome (hand-heart syndrome), Okihiro syndrome, and Wildervanck syndrome.
Continue reading to learn how doctors diagnose Duane syndrome.
Diagnosing Duane Syndrome

When Duane syndrome is suspected, an eye specialist, such as an optometrist or ophthalmologist, will need to obtain a complete family and personal medical history and conduct a full medical and vision exam. The vision exam will include the typical visual acuity tests. Aside from this, the exam will include measuring the misalignment in the eyes, testing the range of movement in both eyes, determining if the patient is using an abnormal head position or turn measuring eyeball retraction and eye-opening size, as well as determining if upshoots or downshoots are also present. In some instances, the eye specialist will recommend the patient to visit their primary doctor or other specialists to rule out disorders connected to Duane syndrome. These exams will typically examine the spine, neck, hands, roof of the mouth, and the patient’s hearing.
Continue reading to learn about the surgical treatment options available to patients with Duane syndrome.
Treatment Through Surgery

Unfortunately, surgery cannot completely fix a patient’s Duane syndrome as it cannot fix the miswired nerves. It can, however, adjust the eye muscles to compensate for the compromised nerves and reduce misalignment, including helping reduce upshoot and downshoot. Surgery can also improve the head turn or abnormal head position (success rate is estimated to be seventy-nine percent or more), and reduce the severity of eyeballs pulling back into the socket when the patient looks in towards their nose. Two examples of surgeries performed are horizontal muscle recession procedures and vertical rectus muscle transposition procedures. The surgery or surgeries chosen depend on the patient and their specific case.
Continue reading to learn about how patients can manage this disorder with lifestyle adjustments.
Treatment Through Lifestyle Adjustments

Although treatment cannot eliminate Duane syndrome, it is vital to manage the condition for the best quality of life. With this in mind, lifestyle adjustments to manage this condition include having special seating in school to help deal with a child’s head turn, installing special rear-view mirrors in the car to assist with driving, and vision therapy to treat the eyes’ inability to turn towards each other or sustain the position. Though uncommon, another treatment is to use a prism on the individual’s glasses to correct a face turn. Treatments for amblyopia, such as the use of an eye patch, may also come into play if this condition is also present with the patient’s Duane syndrome. In all instances, the best advice is to follow the doctor’s orders.