How To Prevent And Treat Peripheral Vascular Disease
Peripheral vascular disease is a disease where the legs, arms, or other body parts receive restricted levels of blood flow. Restricted blood flow happens when the veins or arteries in an individual's limbs become blocked, spasm, or become narrowed. When the peripheral vascular disease is only present in the arteries, it is referred to as peripheral arterial disease. There are two different types of peripheral vascular disease. Organic peripheral vascular disease is precipitated from plaque accumulation, tissue damage, or inflammation. Functional peripheral vascular disease is characterized by a decrease in the flow of blood as a reaction to a mechanism that causes the blood vessels to be inconsistent in size. Symptoms of peripheral vascular disease include peripheral claudication, leg cramps, reddish-blue legs or arms, leg hair loss, slow healing wounds, numbness in the toes, cold skin, thickened toenails, and atrophy.
There are several ways to prevent and treat peripheral vascular disease. Learn about them now.
Get Regular Exercise

Patients can help treat their existing case of peripheral vascular disease if they get regular exercise and make it an ongoing habit. However, individuals who have peripheral vascular disease may lose their ability to mobilize and function the same way they did before developing the condition. An affected individual has been subconsciously wired to avoid exercise due to its association with pain because of peripheral vascular disease. This programming in the brain causes the patient to lose the function of the muscles and circulatory mechanisms in their legs over time. Part of treating peripheral vascular disease is overcoming this mental barrier and working to increase the distance the patient can walk before they begin to experience claudication. Regular exercise is also imperative for treatment because it helps prevent complications that occur as a result of poor circulation and artery occlusion. These complications gangrene, foot ulcers, and even limb amputation. Specialized rehabilitation programs can create an individualized and specific supervised exercise routine for peripheral vascular disease patients that can help them increase the duration of their mobility before claudication onset.
Keep reading to learn more about preventing and treating peripheral vascular disease now.
Eat A Balanced And Healthy Diet

Peripheral vascular disease can both be prevented and treated when individuals eat a balanced and healthy diet that is low in fat and sugar. Peripheral vascular disease can be exacerbated by numerous factors, such as high blood pressure, high cholesterol, and high blood sugar. A healthy and balanced diet that is low in sodium can help decrease blood pressure. High cholesterol is caused by a diet containing too much unsaturated fat. Saturated fats are beneficial because they help increase the amount of good cholesterol in the body, which lowers the amount of plaque-forming cholesterol. A diet that is too high in unsaturated fats is also associated with obesity and excess adipose tissue, which contributes to inflammation and increased blood volume in the body, resulting in further blood vessel damage. A diet low in sugar can help decrease the risk of developing diabetes, which also contributes to peripheral vascular disease symptoms.
Get more details on treating and preventing peripheral vascular disease now.
Manage Blood Sugar

Regardless of prediabetic or diabetic status, an individual can help prevent the development of peripheral vascular disease if they manage their blood sugar. Diabetes patients are at an increased risk of developing peripheral vascular disease because of several malfunctions that occur as a result of high blood sugar. Individuals with diabetes experience dysfunction of the endothelial tissues inside of the blood vessels, hypercoagulability of the blood, dysfunction of the vascular smooth muscle cells, and increased levels of inflammation in the body. Early intervention in type 1 diabetes patients can help improve the prognosis of long term diabetes management, lowering the general risk of developing atherosclerosis and peripheral vascular disease. The systemic form of atherosclerosis is more common in type 2 diabetes because it goes undiagnosed and unmanaged for a longer duration than type 1 diabetes. High blood sugar causes the blood to have a harder time flowing through the blood vessels and can cause high blood pressure and inflammation that also contribute to the development of peripheral vascular disease.
Read more about treating peripheral vascular disease now
Medication

Peripheral vascular disease patients may need to be treated with medication to help increase blood flow to the affected areas of the body. For some patients, changes in lifestyle habits may be sufficient for treatment. However, it is not enough for everyone. A peripheral vascular disease patient may need to take antiplatelet medications to reduce the ability of the platelets to stick together and develop blood clots. Anticoagulant medications may need to be taken to slow down the clotting cascade and impede the formation of blood clots. Statins can help lower a patient's cholesterol, which can help prevent further occlusion of the blood vessels in the lower extremities that cause peripheral vascular disease symptoms. Cilostazol is a medication peripheral vascular disease patients to dilate the blood vessels and help them walk a longer distance before experiencing claudication. Hypertension-controlling drugs are also commonly used to decrease the chances of further blood vessel damage.
Discover additional treatments for peripheral vascular disease now.
Angioplasty
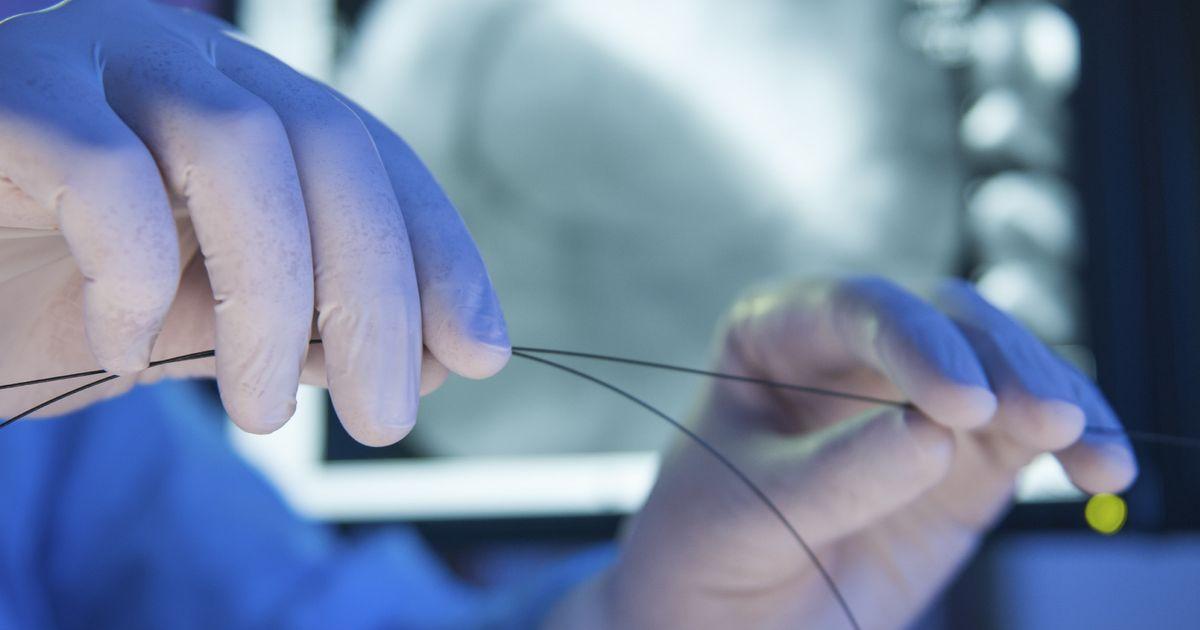
Peripheral vascular disease patients may need to undergo a minimally invasive procedure referred to as an angioplasty as part of their treatment plan. Angioplasty and percutaneous transluminal angioplasty are terms used to describe a procedure where a blocked or narrowed artery can be widened. This mechanism is accomplished by the use of a catheter or a long, thin tube equipped with a small balloon at the end. The catheter is threaded into an artery in the patient's groin or arm, and maneuvered to the site of the narrowed artery. Once there, the surgeon inflates the balloon to expand the inner space of the affected artery. A stent or wire mesh tube shaped like a cylinder may or may not be inserted and installed during the angioplasty to help hold and keep the narrowed artery open. Angioplasty is utilized in patients who experience excessive claudication that puts extreme limits on their daily activities and has not been able to be successfully treated with other measures like lifestyle changes, exercise, and medications.