How To Treat And Prevent Thoracic Outlet Syndrome
Thoracic outlet syndrome develops when blood vessels and nerves within the thoracic outlet (the space between the collarbone and first rib) are compressed. The syndrome can be caused by car accidents, repetitive strain related to sports or occupations, and pregnancy. Patients who have an extra rib or other anatomical differences may be at an elevated risk of this condition. Symptoms of thoracic outlet syndrome typically include pain, numbness, and tingling in the hands, arms, shoulders, and neck. In cases where veins or arteries are compressed, patients may also exhibit cold hands, pale or bluish fingers, a weak pulse in the arm, and weakness in the arms and hands. A lump may be present near the collarbone. To diagnose this condition, doctors use a combination of physical examination, x-rays, CT and MRI scans, ultrasounds, and nerve conduction studies. The doctor will move the patient's neck, arms, and shoulders in various ways to check for pain or loss of flexibility. Some patients may need to have a scalene muscle block, arteriogram, or venogram to confirm the diagnosis. These tests can be useful in planning the most appropriate treatment for the patient's needs.
The methods outlined below are beneficial in the prevention and treatment of thoracic outlet syndrome.
Clot-Dissolving Medication

Clot-dissolving medication, also known as thrombolytic medicine, is typically required for cases of thoracic outlet syndrome that compress the veins and arteries. Compression of these vessels may lead to dangerous blood clots, and clot-dissolving medication can be useful in breaking up these clots and preventing complications. Medicines that dissolve clots are normally given intravenously in the hospital, and they are only administered within a certain time frame after the discovery of a clot. Alteplase, urokinase, and reteplase are some examples of frequently used thrombolytics. The main risk of these drugs is serious, excessive bleeding, and patients are monitored closely while the medicines are administered. If the clot is successfully dissolved, doctors will also prescribe anticoagulants (blood thinners) for patients to take at home to prevent future blood clots from forming.
Uncover more treatments for thoracic outlet syndrome now.
Physical Therapy

Physical therapy is often the first treatment doctors recommend for patients who have thoracic outlet syndrome that involves nerve compression. The physical therapist teaches the patient stretches and exercises that improve range of motion in the upper body and open up the thoracic outlet. The exercises build strength in the shoulders and promote a balanced posture. When performed frequently and with proper technique, physical therapy exercises may reduce some of the pressure on the blood vessels and nerves within the thoracic outlet. Typically, the majority of the exercises use the patient's own body weight, and elastic bands may make it easier to perform certain stretches. When choosing a physical therapist, patients might wish to look for one who specializes in thoracic outlet syndrome. If any of the exercises cause an increase in pain or result in the development of other worrying symptoms, patients should let their physical therapist know. They may also wish to consult their healthcare provider to ensure no additional damage has been done.
Continue reading to reveal more methods of treating thoracic outlet syndrome effectively now.
Thoracic Outlet Decompression

Thoracic outlet decompression is a surgical procedure that may be considered for patients who have not improved with conservative treatment. The operation is performed with general anesthesia, and it can be completed with several surgical techniques. In the transaxillary technique, surgeons remove part of the first rib through an incision in the chest without disturbing the surrounding vessels or nerves.
Some surgeons will choose to use a supraclavicular method for the procedure. This involves making an incision just underneath the neck to expose the brachial plexus. The surgeon examines this area for trauma, and they might opt to remove muscles contributing to the compression. If needed, removing the first rib entirely can provide an additional reduction in compression. For cases in which extensive repair is required, an infraclavicular method may be used to repair compressed veins. This method requires a long incision underneath the collarbone and across the chest.
Learn more about how to treat thoracic outlet syndrome now.
Take Frequent Breaks

To prevent and treat thoracic outlet syndrome, it is essential for patients to take frequent breaks. Repetitive movements of the upper body that are required for certain jobs and sports are one of the major causes of this syndrome; thus, taking frequent breaks to rest from these repetitive motions may help prevent the development of the syndrome, and breaks can reduce pain for individuals who already have the condition. Ideally, patients should take a break at least once every twenty to thirty minutes. During the break, the muscles of the upper body should be completely relaxed, and patients may wish to try some gentle stretches to reduce stiffness. It can be helpful to change positions several times during a break, and patients might want to consider using cushions or other soft items to rest their arms, shoulders, and neck while on a break. Recording the amount and duration of breaks in a symptom diary can be beneficial. If patients determine they are taking sufficient breaks but still experience pain, a clinician should be consulted.
Get more details on thoracic outlet syndrome treatment options now.
Practice Good Posture
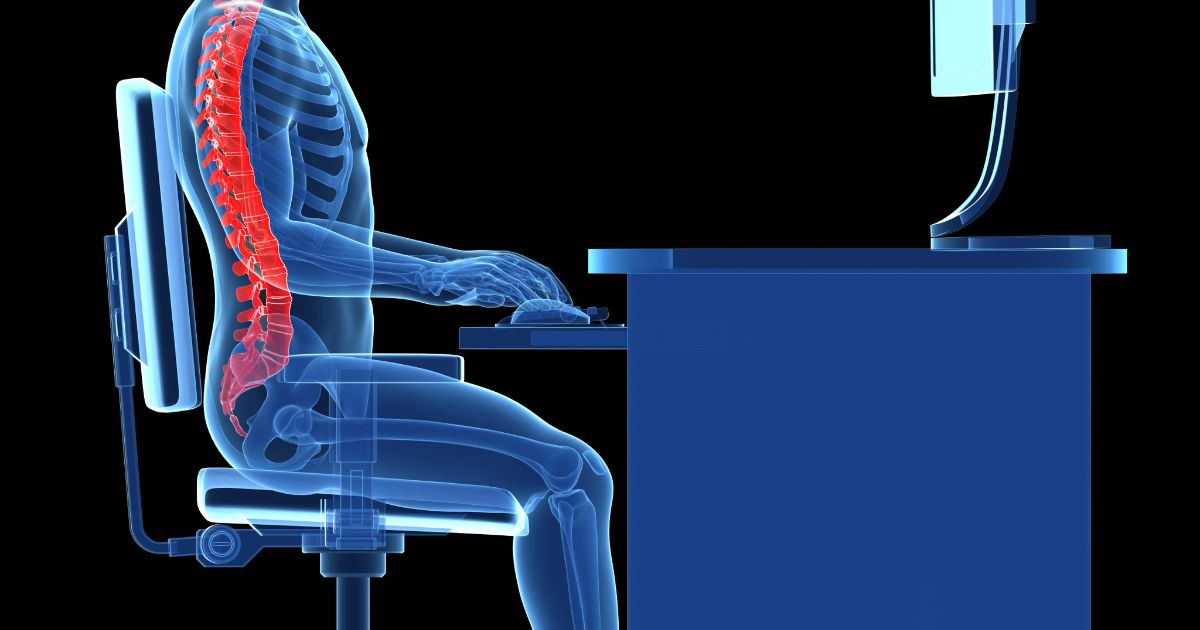
Doctors and physical therapists suggest individuals practice good posture as a method of preventing thoracic outlet syndrome. Good posture is one in which the body is properly aligned and balanced so undue stress is not placed on any one muscle group or nerve. To promote good posture, patients can invest in ergonomic desk chairs that reduce strain on the back. It can also be useful to purchase computer desks that are height-adjustable and capable of tilting to alleviate hand and nerve pain from typing. At home, a firm mattress or an adjustable bed may promote a balanced sleeping pose, and this could reduce the risk of further injury. Due to anatomical differences, a balanced posture may look slightly different for each individual. Patients who have questions about what proper alignment looks like for them can get advice from a physical therapist, sports medicine physician, or orthopedist.