Ways To Treat And Prevent Osteomyelitis
Osteomyelitis is a rare bone infection that affects only two in every ten thousand individuals on an annual basis. Bones may become infected if bacteria migrate from another infected area of the body to the bones or if an individual experiences a compound fracture. Infection can also occur in those who have had surgery, especially those involving knee and hip replacements. Staph infections cause most incidences of osteomyelitis. While the majority of osteomyelitis cases are attributed to individuals with diabetes or those with compromised immune systems, such as with HIV or AIDS, sickle cell anemia and rheumatoid arthritis have an increased risk of developing osteomyelitis as well. Get to know the major treatment options now.
Surgery

In cases of severe osteomyelitis, surgery may be required to eradicate the current infection and prevent it from spreading. There are several surgical procedures a physician can use to treat osteomyelitis. For instance, surgeons may opt to open the bone and drain the area of any infected fluid. In some cases, debridement is the best option. Debridement involves the removal of the infected areas of the bone, and sometimes tissue, as well as a small portion of the healthy bone. The removal of the healthy bone helps to guarantee there is no remaining infection residing within the bone. In severe cases, when other methods fail to work, a physician may have no other option but to amputate the limb to prevent the spread of osteomyelitis to other areas of the body.
Continue reading to reveal more ways to treat this condition.
Infection Treatment

In the beginning stages of osteomyelitis, physicians will typically order a biopsy of the bone to determine which bacteria is attacking it and begin infection treatment. A biopsy involves the removal and examination of diseased tissue, and once the bacteria is identified, treatment for the infection can be assessed and implemented accordingly. Infection treatment assists the compromised immune system in fighting the invading bacteria. Depending on the severity of the osteomyelitis, a physician may recommend treatment either orally or intravenously. Intravenous treatment is typically given first and may need to be administered for four to six weeks.
Keep going to understand more ways in which osteomyelitis is treated.
Proper Wound Care

The best way to avoid contraction of osteomyelitis is to engage in proper wound care, as even a small cut can evolve into osteomyelitis if it is not treated properly. It is important to make sure to clean wounds thoroughly and ensure they are covered with sterile bandages. When changing bandages, individuals should make sure to wash their hands and the surrounding wound area properly. If symptoms of infection do occur, such as swelling, pain to the touch, and redness, it is important to make an appointment with a physician as soon as possible. Large, deep wounds and any injuries to the bone should be examined by a medical professional right away.
Get to know the next treatment option for osteomyelitis now.
Needle Aspiration
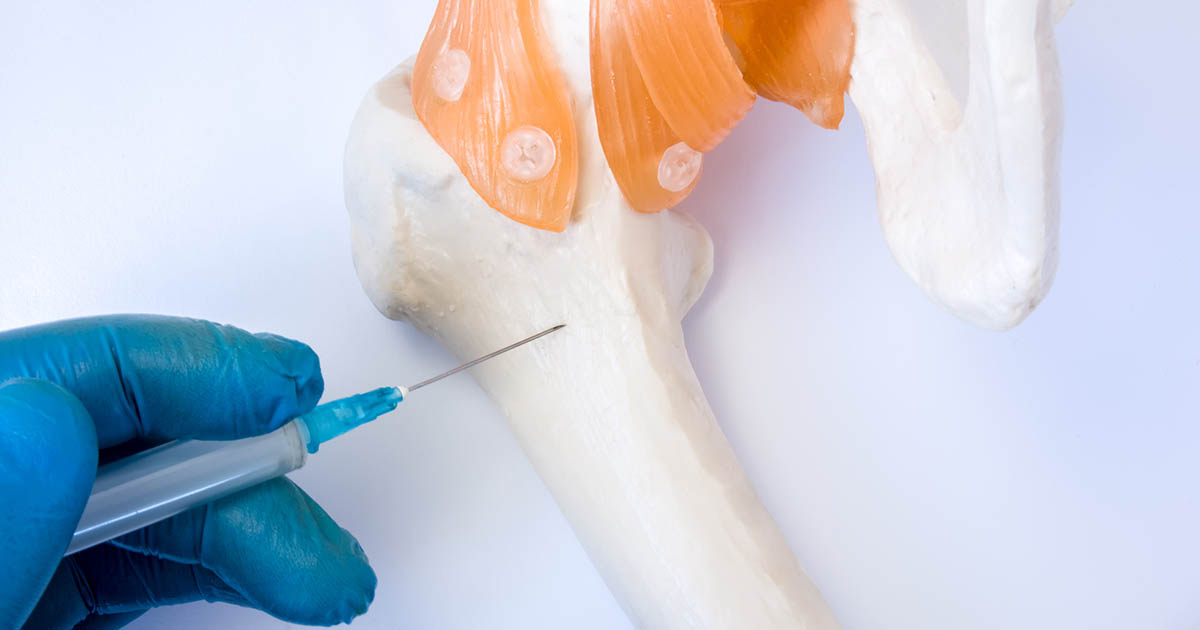
Similar to a general biopsy, a needle aspiration involves the removal of infected tissues and fluid at the infection site so doctors can determine the type of bacteria infecting the bone. However, unlike a general biopsy, which requires a patient to undergo general anesthesia, a needle aspiration involves the use of a local anesthetic agent to numb the nerve endings in the area of the infection and does not require a patient to be put to sleep or an incision. Instead, a long needle is inserted into the patient's body through skin and tissue and directly into the bone to extract the infection. This type of procedure is considered less invasive and is usually safer for the patient.
Learn about more treatments for osteomyelitis now.
Prosthesis Replacement
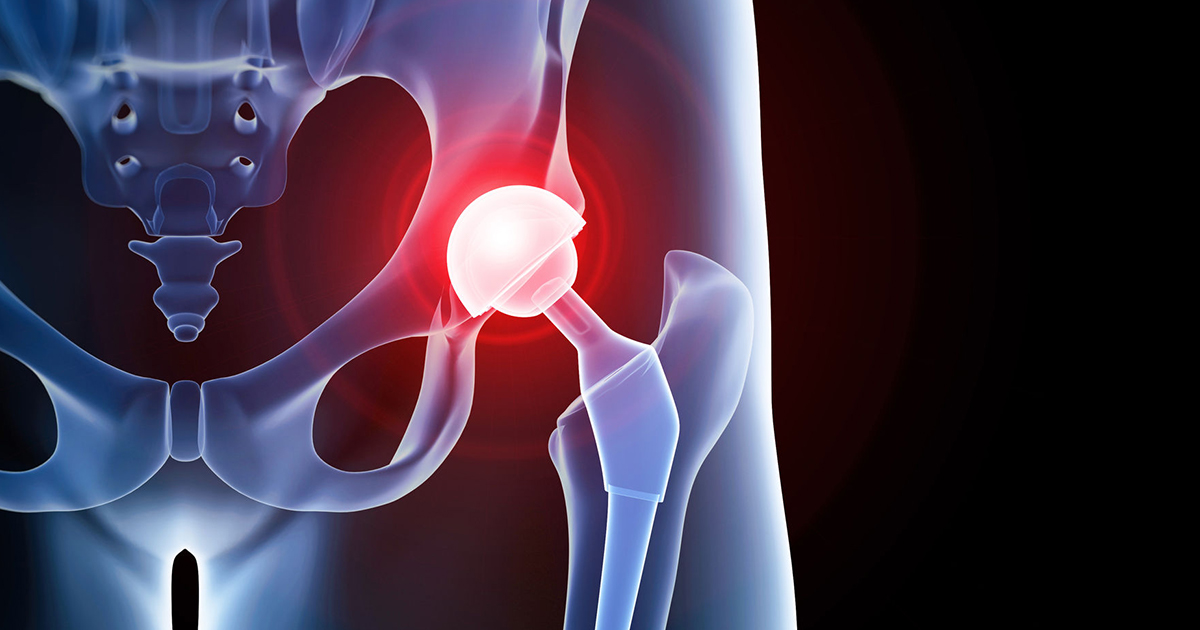
Individuals with prosthetic limbs and joints have an increased risk of developing infections and those with prosthetics, such as steel rods or screws placed into the bone following a compound fracture, should be particularly aware of the signs of osteomyelitis. The increased risk stems from the fact most prosthetics placed in the body are metal, and the immune system is unable to deliver white blood cells to the prosthetic to fight off infection. Osteomyelitis infections can be recurring, and when consistent recurrences of infection occur in a prosthetic limb, it may be necessary to remove the prosthetic and get a prosthesis replacement. The procedure would involve placing the individual under general anesthesia to extract the infected prosthetic. In some cases, if the bone has re-aligned or completely healed, there will be no need to insert a new prosthetic.